Vitamin D and the immune system
How much vitamin D3 to take, according to body weight and obesity status: #00-how-much.
This page cites and discusses the most pertinent research on vitamin D and the immune system. Topics include:
- 25-hydroxyvitamin D to calcitriol based intracrine
signaling (sometimes incorrectly referred to as "autocrine") inside a
single immune cell. A related paracrine signaling system affects
the behaviour of nearby cells.
All medical professionals and immunologists need to
understand these cellular signaling systems, but few do, in part because the vitamin D research
literature does not explain them clearly.
- The need to attain at least 50 ng/mL (125 nmol/L) circulating
25-hydroxyvitamin D which is required for full immune function.
Most people have half or less of the 25-hydroxyvitamin D they need to
be healthy.
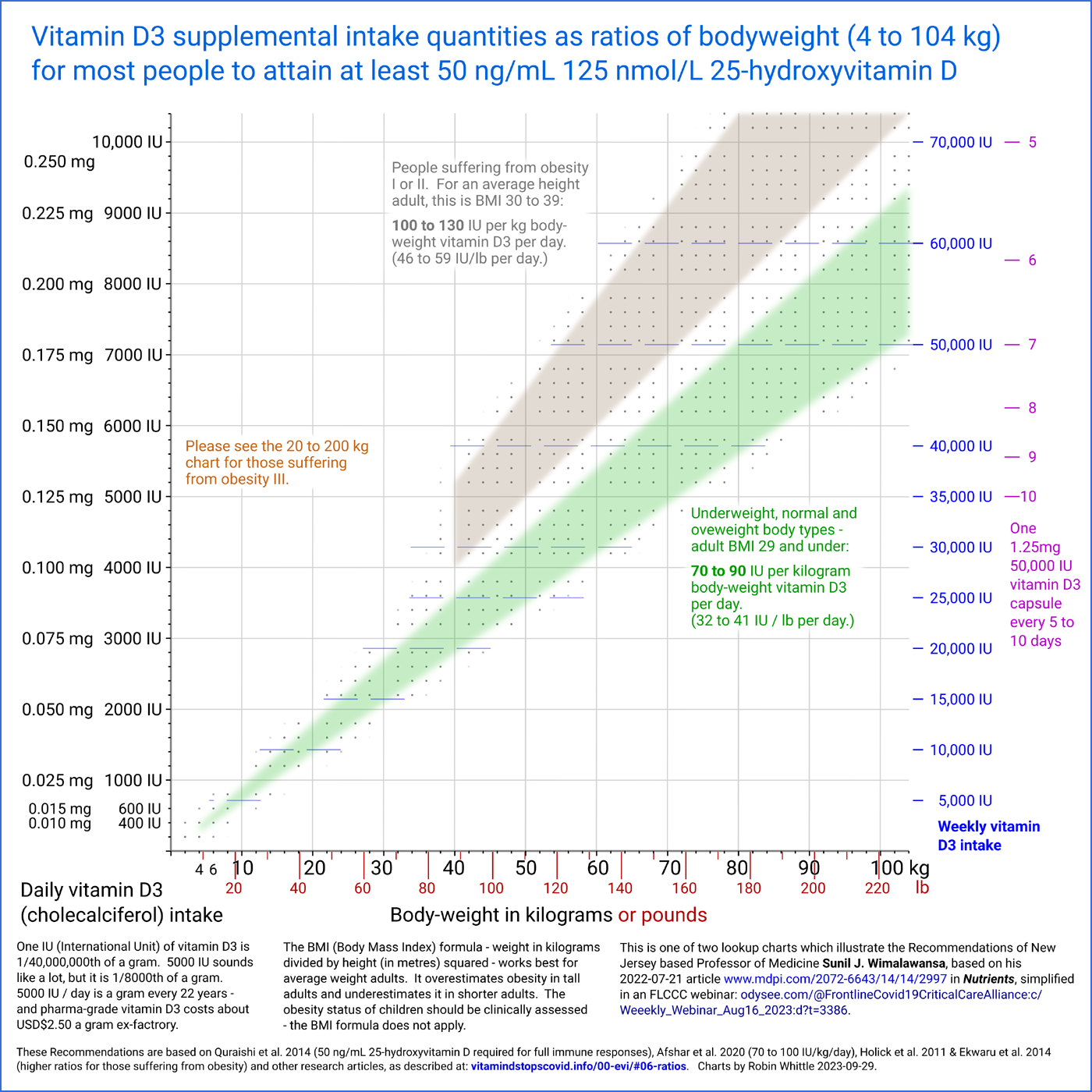
- Vitamin D3 supplemental intake quantities as
ratios of bodyweight - with higher ratios for those suffering from
obesity.
- The importance of such good 25-hydroxyvitamin D levels to treat or
prevent numerous acute and chronic diseases, and to facilitate good
health starting from early pregnancy and for all of life, including to
reduce the incidence of neurodegeneration in old age.
This is an updated version of a submission to the UK Office for
Health Improvement & Disparities call for evidence (2022-04-03):
However, they never received it. This submission was written by Robin Whittle and co-signed by Patrick W. Chambers, MD.
Latest update: 25 November 2024 (First established 2022-05-15. See Update Notes at end: #updates.)
Robin:
I am an electronic technician and C++ computer programmer. I have
been raising awareness of the need for proper vitamin D3
supplementation, most urgently to suppress COVID-19 transmission, harm
and death, since late March 2020. I live in Daylesford, NW
of Melbourne, Victoria, Australia. I was born in Wantage, in
1955, so I am a UK citizen. I have no formal qualifications in
any field.
I asked
Patrick to read my
submission, hoping he would support it. He did so and asked to be
a co-signer. So the submission is from both of us, though I (RW)
wrote it.
Patrick gained his Bachelor of Arts at Princeton University in 1971,
specializing in Mathematics. He studied Medicine at University of
California, Davis and after graduating in 1975 studied at the LA County/USC Medical Center,
gaining a degree in Anatomic and Clinical Pathology (board
certified) in 1979.
From 1979 he worked in the Department of Pathology, Torrance Memorial
Medical Center, in California, mainly as Managing Director. He
retired and moved to Hawaii in 2004. His research interests
www.researchgate.net/profile/Patrick-Chambers-4/ include vitamin D, magnesium and other nutrients.
Patrick and I are members of the Nutrition for Immune System Health (NISH) email discussion list: nish.groups.io.
If you find the articles cited in this submission seriously
interesting, you might like to join us and the other researchophiles on
the NISH list.
To find vitamindstopscovid.info easily, go to 5nn.info
(search for "5 neglected nutrients"), where there are links to this
vitamin D material, and a printable PDF of my vitamin D flyer.
../ To the main page of this site.
Robin Whittle rw@firstpr.com.au Daylesford, Victoria, Australia.
Twitter: twitter.com/RobinWhittle3 Substack: nutritionmatters.substack.com
May 2023 Article at Brownstone.org
For a briefer account of much of the following material, plus a discussion of
Dror et al. 2022,
which contains excellent information on how low pre-infection
25-hydroxyvitamin D levels are associated with, and surely to a large
extent cause, severe symptoms and death due to COVID-19:
please see the article Simon Goddek and I wrote for the Brownstone Institute:
This has an English robotic voice narration and text translations into 18 other languages. Comments and discussion:
nutritionmatters.substack.com/p/vitamin-d-and-the-immune-system-article .
Contents
| Link
|
Description
|
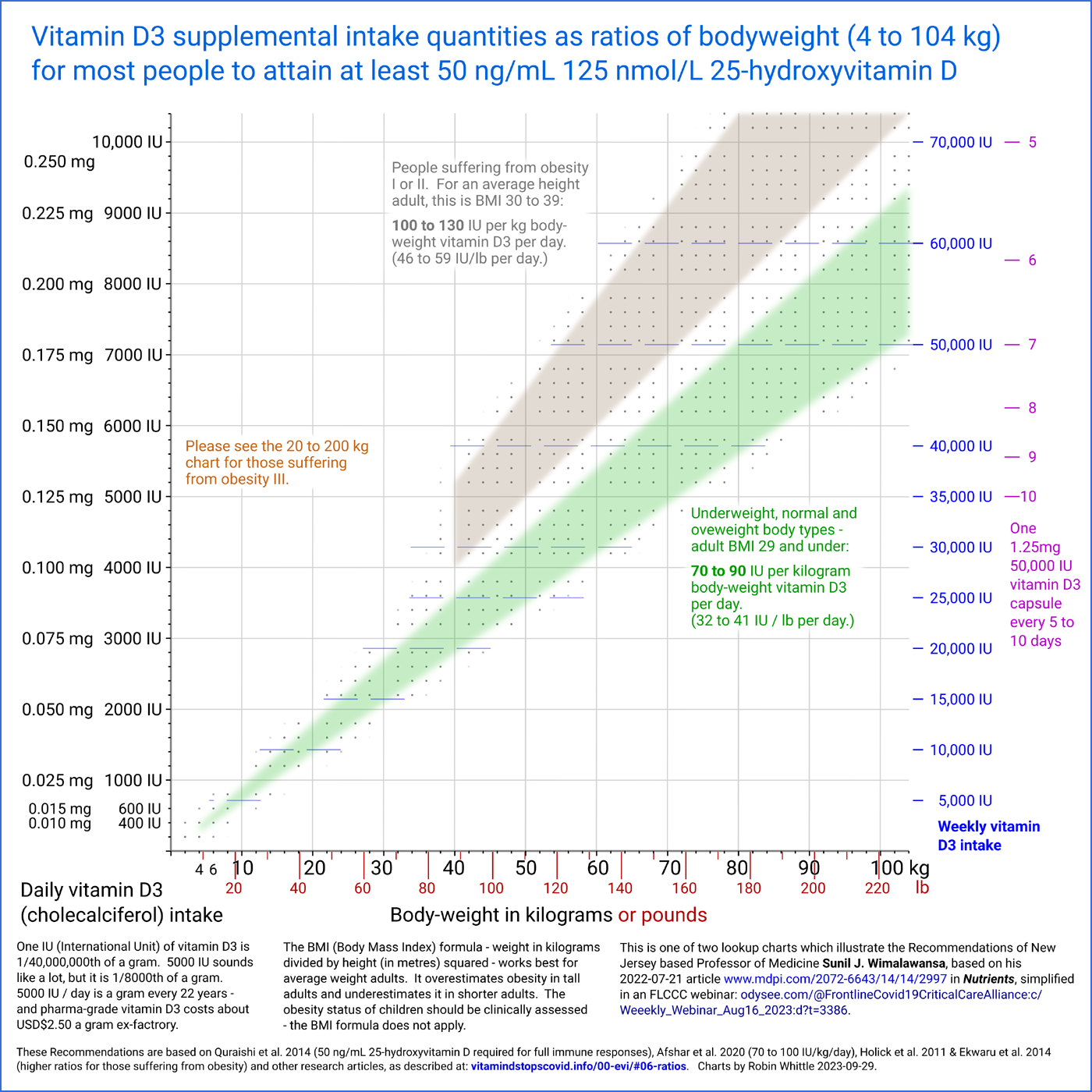
#00-how-much
|
How much vitamin D to take.
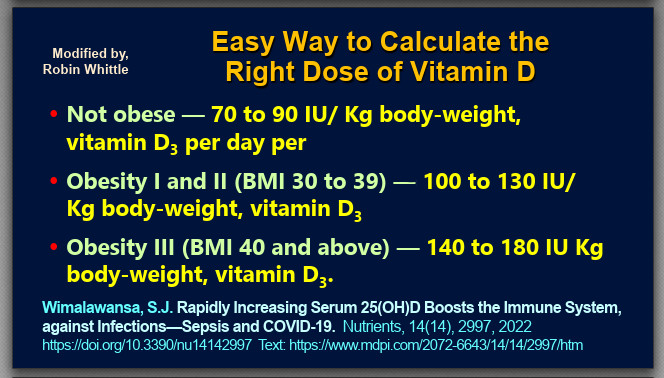
Prof. Sunil Wimalawansa's (simplified somewhat in 2023)
recommendations, according to body weight and obesity status, based on
his 2022 Nutrients article: Rapidly Increasing Serum
25(OH)D Boosts the Immune System, against Infections - Sepsis
and COVID-19. See also: nutritionmatters.substack.com/p/how-much-vitamin-d3-to-take
|
#00-50ngmL
|
At least 50 ng/mL (125 nmol/L) circulating 25-hydroxyvitamin D is needed for proper immune function. The Massachusetts General Hospital research which shows this most clearly.
|
#01-intro
|
Introduction.
|
| #02-compounds
| Vitamin
D3 cholecalciferol, 25-hydroxyvitamin D calcifediol and
1-25-dihydroxyvitamin D calcitriol.
Tutorial explanation of
25-hydroxyvitamin D >>> calcitriol intracrine and paracrine signaling. These are completely different from hormonal (endocrine) signaling.
|
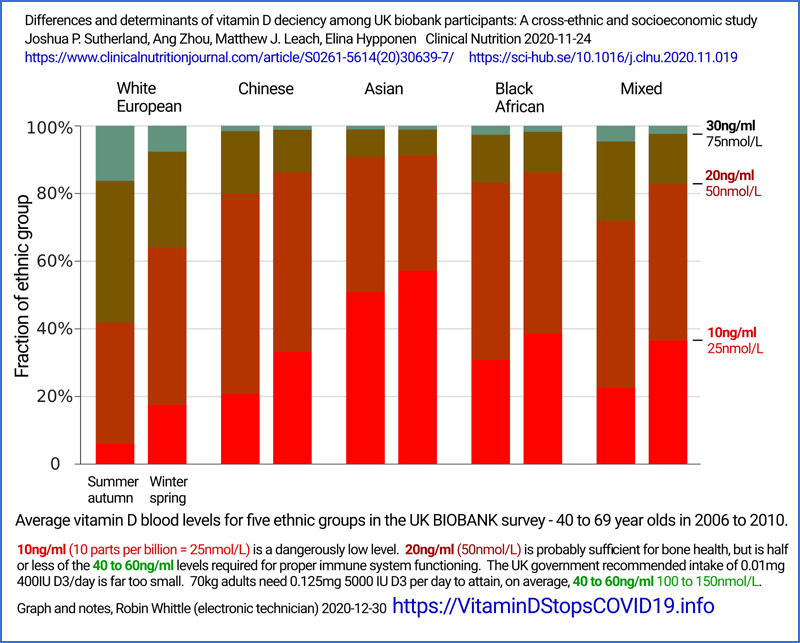
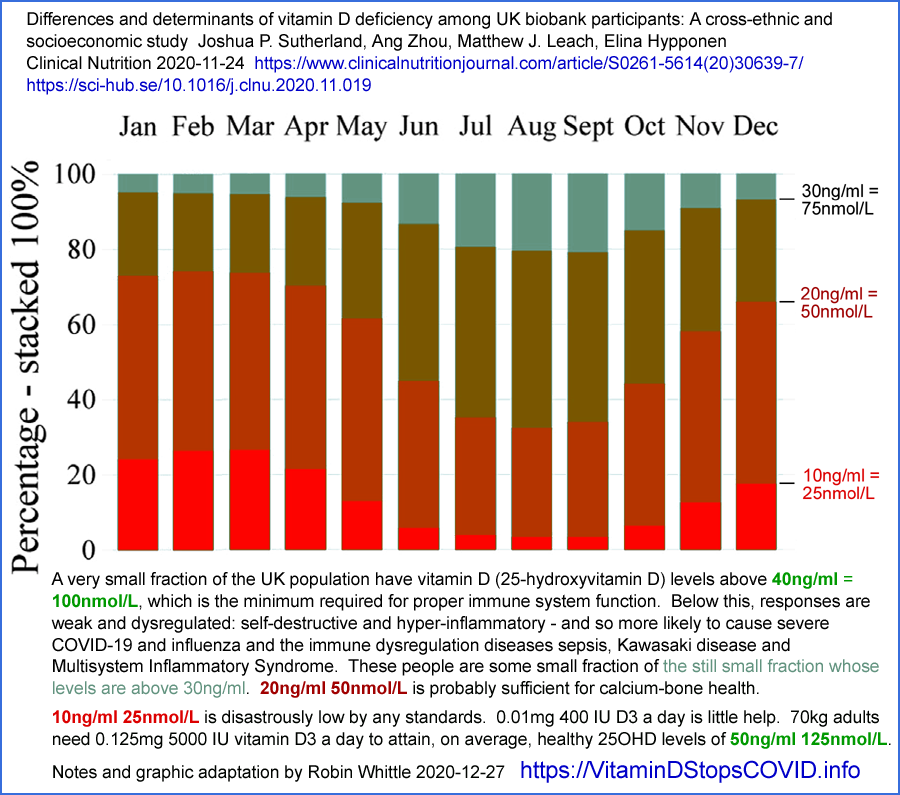
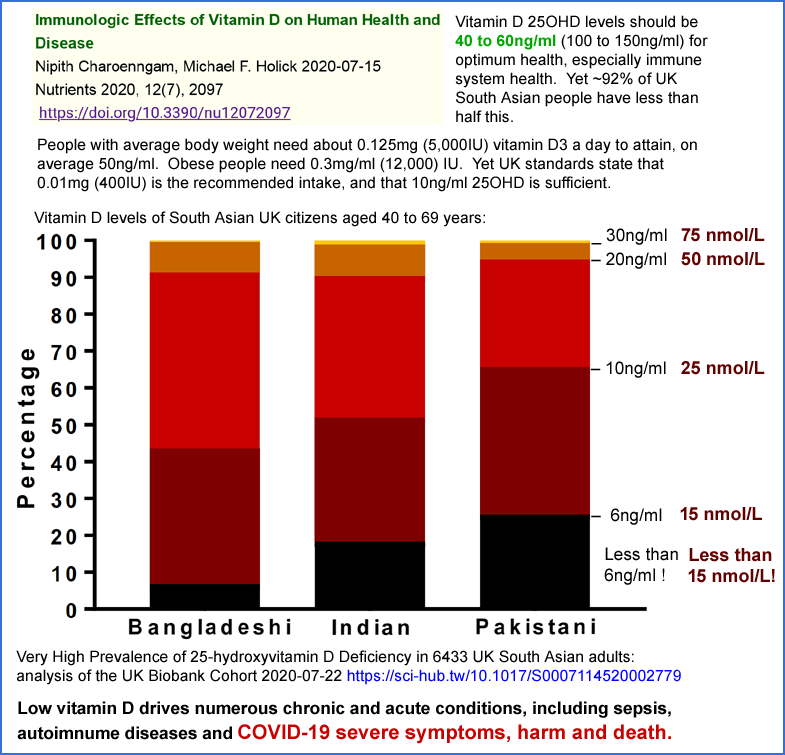
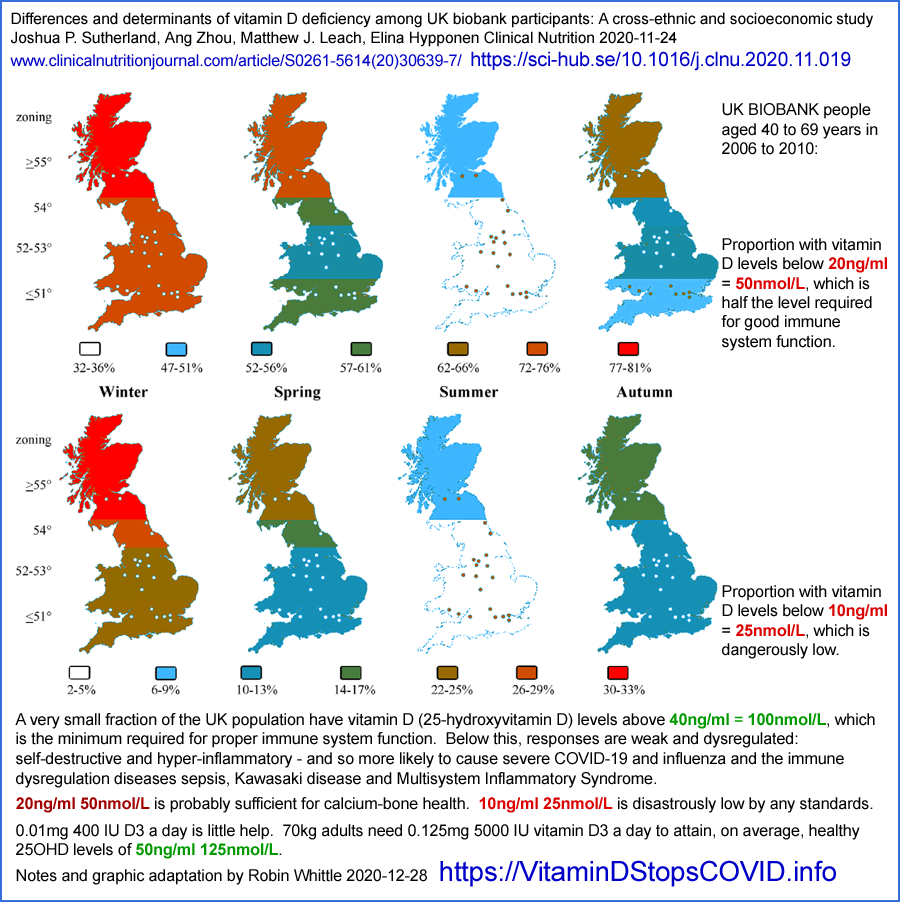
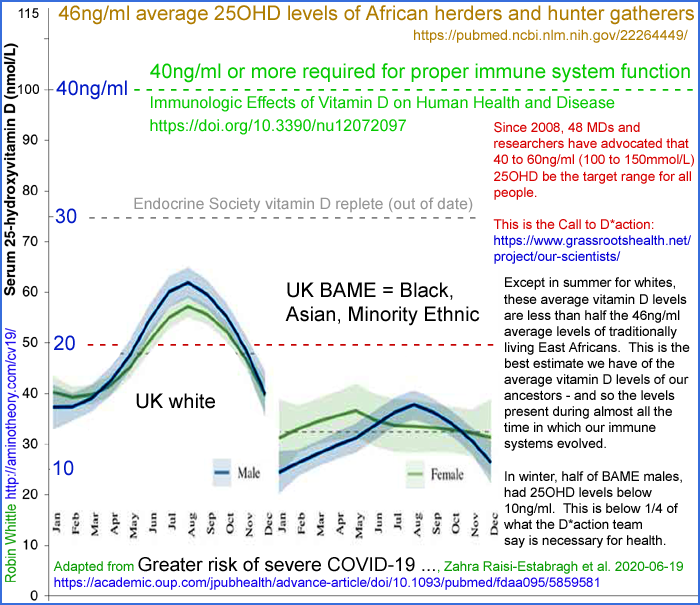
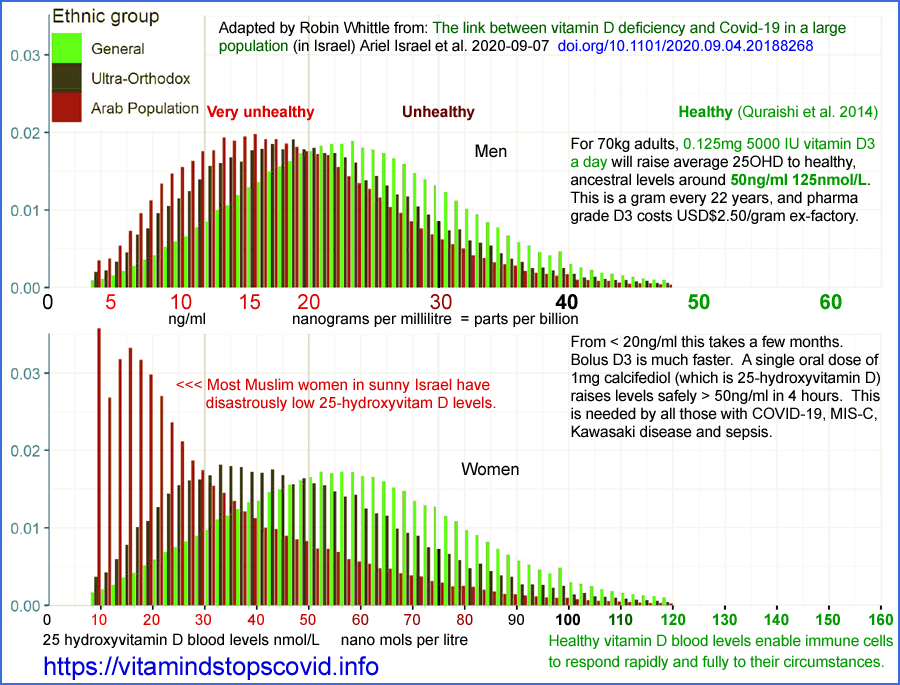
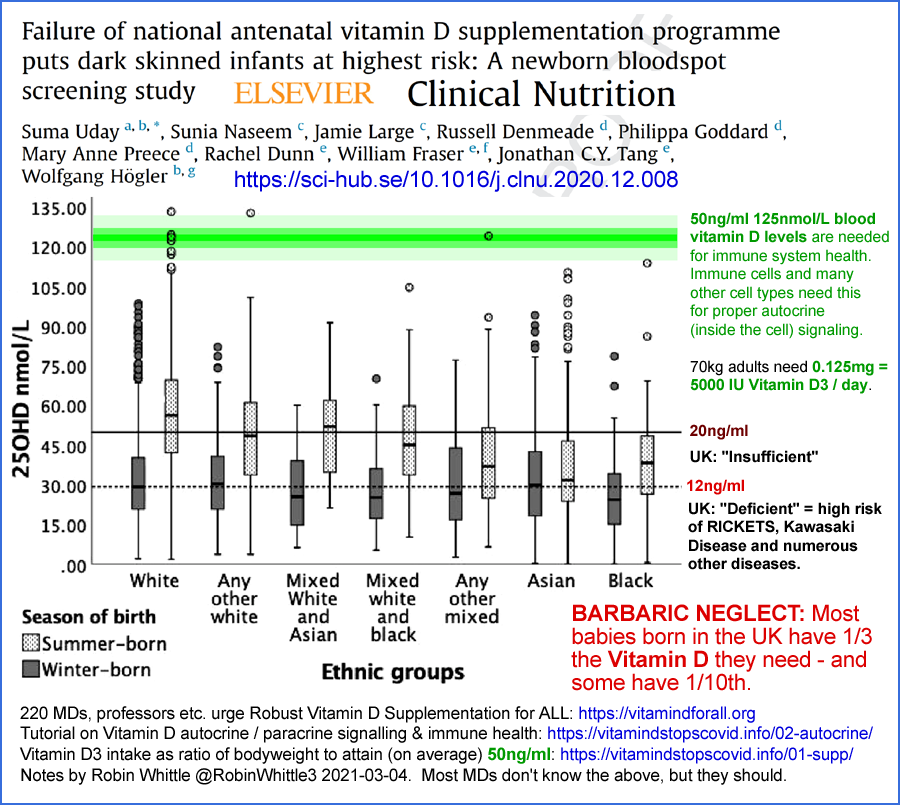
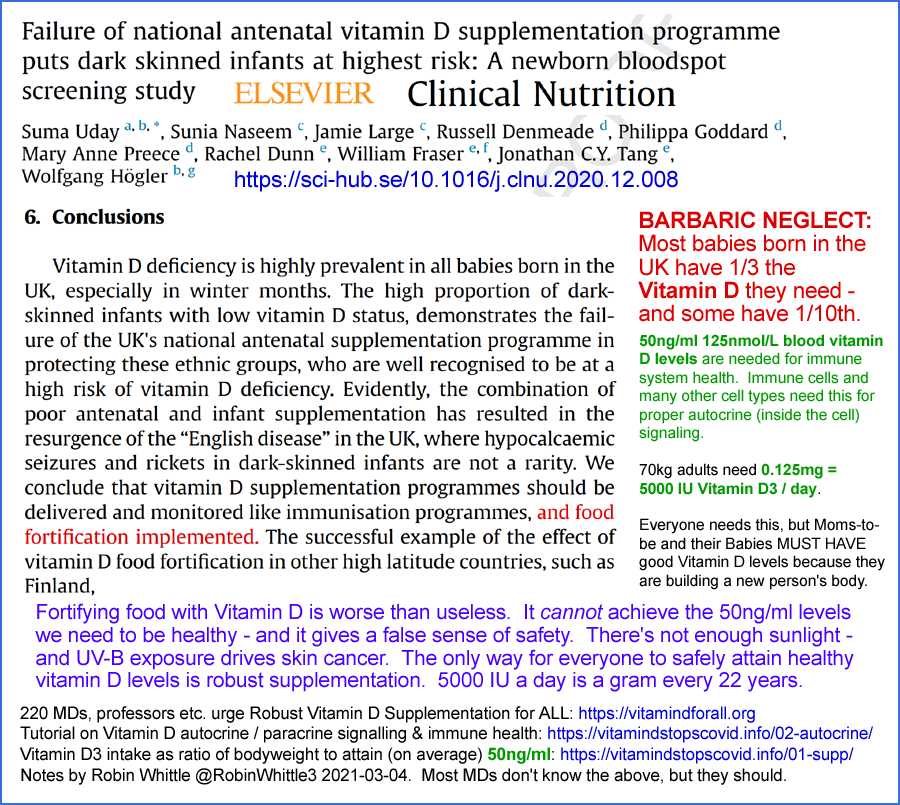
| #03-uk-low
| Terribly low 25-hydroxyvitamin D levels, especially in the UK.
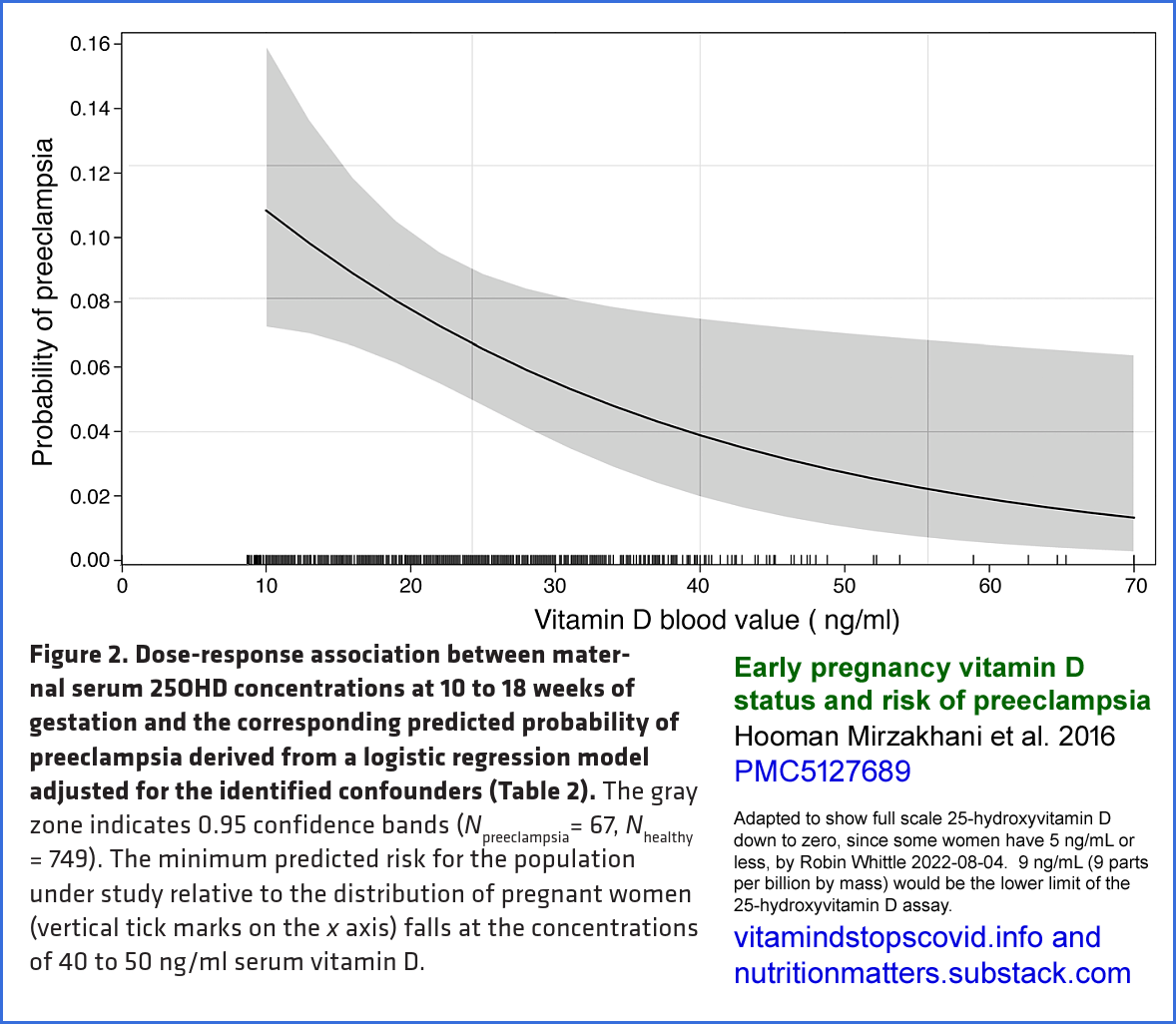
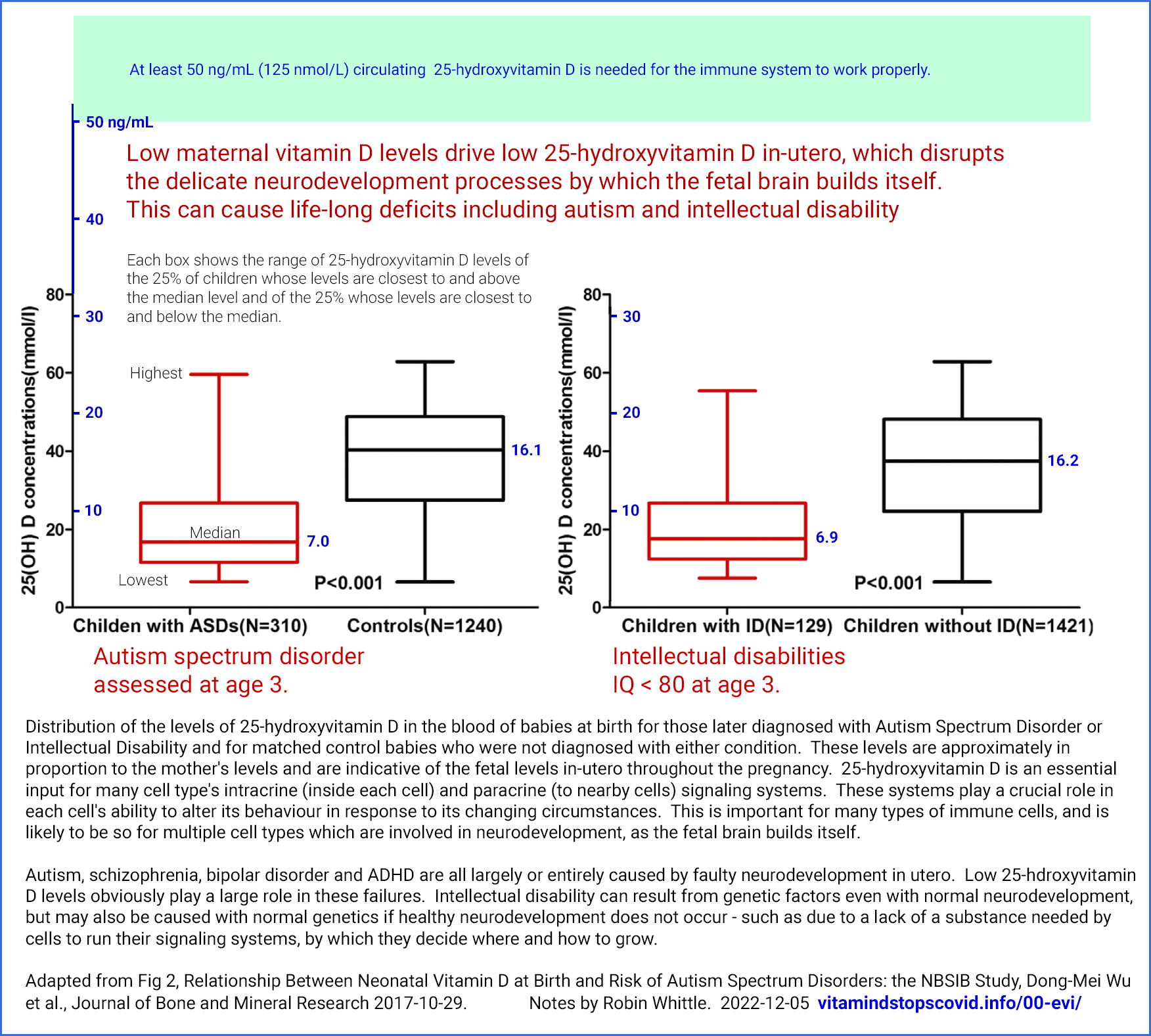
This includes a section #3.2 on low in-utero
25-hydroxyvitamin D levels causing (or strongly contributing to)
autism, intellectual disability and other neurodevelopment disorders
such as schizophrenia and ADHD. This section also concerns low birth
weight and pre-eclampsia.
A section #3.3 concerns low
25-hydroxyvitamin D levels causing neurodegenerative diseases including
Parkinson's disease, and evidence that raising 25-hydroxyvitamin D
levels sufficiently slows or halts disease progression - with some
evidence that lost motor control faculties can be recovered.
|
| #04-health
| The need for 50 ng/mL (125 nmol/L) 25-hydroxyvitamin D.
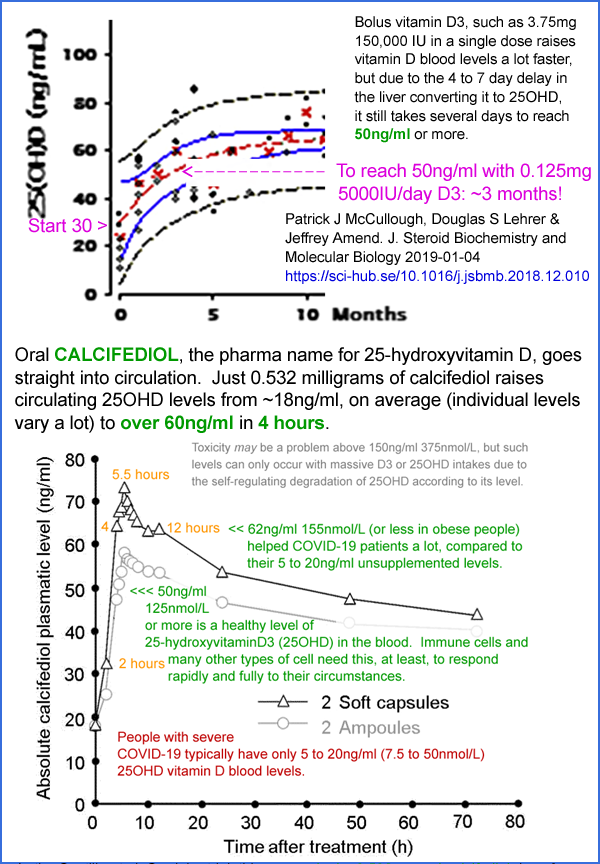
For clinical emergencies, see #4.7 regarding using a single oral dose of about 1 milligram of calcifediol (which is
25-hydroxyvitamin D) for 70 kg bodyweight, to raise the patient's
25-hydroxyvitamin D level safely over 50 ng/mL in about 4 hours.
If this is not available, 10 mg 400,000 IU vitamin D3 should be used,
which will take about 4 days to raise the level as needed for the
immune system to work properly.
|
| #05-history
| The UK government's current vitamin D recommendations are based on the erroneous 2011 US/Canadian Institute of Medicine report.
|
| #06-ratios
| How the vitamin D3 supplemental intake quantities as a ratio of body-weight used at the start of this page #00-how-much. were derived and developed.
|
| #07-fortif | Fortifying food with
vitamin D3 can only provide a small fraction of what people need for full immune system function.
Government efforts should be directed entirely at facilitating proper
supplementation. |
| #08-misinf |
The
UK government misinforms the public about the adequacy of fixed,
excessively small, supplemental intakes of vitamin D3 and about intakes
greater than 0.1mg 4000 IU / day being potentially harmful. |
| #09-role |
The best ways governments can support their citizens regarding vitamin D. |
#sjw-updated-ratios
00 How Much Vitamin D to take?
25-hydroxyvitamin D in the bloodstream
is produced in the liver from vitamin D3 cholecalciferol which is ingested or created
in the skin by ultraviolet B light exposure of ideally white
skin. This circulating 25-hydroxyvitamin D is used by the kidneys
and
immune cells. This is what is tested in "vitamin D" blood tests.
As explained below, there is very little vitamin D3 in food.
There's no such thing as a "vitamin D rich food" in terms of being able
to attain the
50 ng/mL (125 nmol/L) or more level of 25-hydroxyvitamin D which the immune system needs to function properly.
Food which is fortified with vitamin D3 cannot provide what we need for proper immune system function. See:
#07-fortif below.
Ultraviolet B light exposure of ideally white skin, with no glass, sunscreen or clothing barriers, can produce enough vitamin
D3 to attain at least 50 ng/mL circulating 25-hydroxyvitamin D, but to
rely on this would require UV-B exposure all year round. Far from
the equator, such UV-B is only available naturally in the middle of
cloud-free summer days. All such UV-B exposure damages DNA and so
increases the risk of skin cancer.
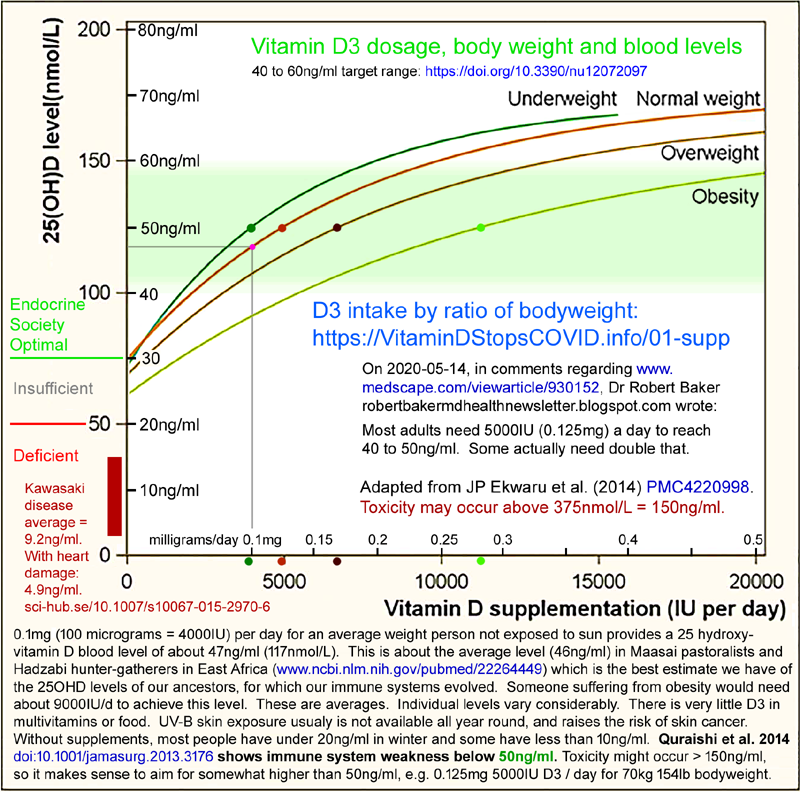
Fortunately, supplemental vitamin D3 is inexpensive and the quantities
required are very small. It can be taken every day, or in larger
amounts once every week to ten days. As the ingested vitamin D3
is hydroxylated in the liver, it takes a few months to build up
25-hydroxyvitamin D levels in the bloodstream to the desired level of
at least 50 ng/mL (1 part in 20,000,000 by mass).
Although vitamin D has been researched since 1923, there is only one peer-reviewed article which recommends
how much vitamin D3 to take, to attain at least 50 ng/mL circulating 25-hydroxyvitamin D, without the need for blood tests or medical monitoring,
for people of all ages, all body weights and all body types
- from underweight to obese. This is New Jersey based
Emeritus Professor of Medicine, Dr Sunil J. Wimalawansa's article in
Nutrients, cited
below
#sjw-article.
The Recommendations in that article are rather complex. In a
webinar with Dr Paul Marik for the
COVID-19 Front Line Critical Care Consortium, on 16
August 2023:
at 56:26,
Prof. Wimalawansa presented a simpler version of his recommendations for
how much vitamin D3 to take, per day, on average, as ranges of ratios of body weight:
Here are his recommendations for average daily vitamin D3 supplemental quantities:
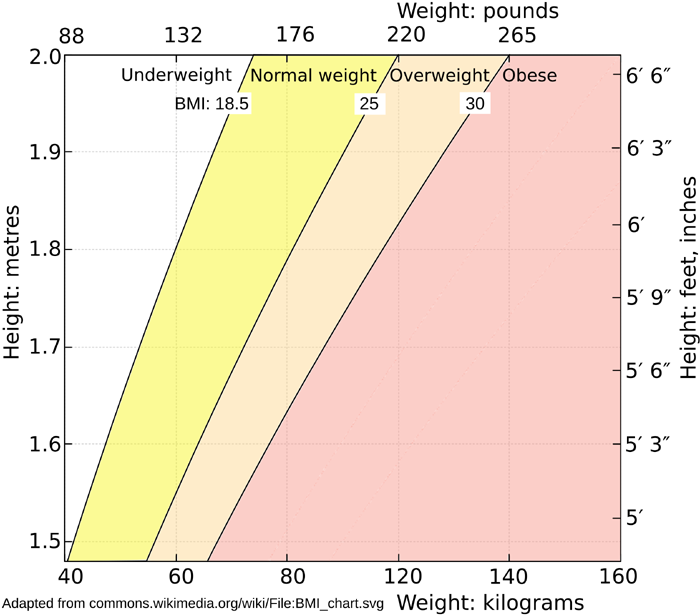
70 to 90 IU / kg body weight for those not suffering from obesity
(BMI < 30).
100 to 130 IU / kg body weight for obesity I & II (BMI 30 to
39).
140 to 180 IU / kg body weight for obesity III (BMI > 39).
For those who think in pounds, divide by 2.2:
32 to 41 IU / pound - no obesity
46 to 59 IU / pound - obesity I and II
64 to 82 IU / pound - obesity III
For countries which use micrograms (1/1,000,000 gram, "mcg" in medicine, which is 40 IUs):
1.8 to 2.3 mcg / kg - no obesity
2.5 to 3.3 mcg / kg - obesity I and II
3.5 to 4.5 mcg / kg - obesity III
0.8 to 1.0 mcg / pound - no obesity
1.1 to 1.5 mcg / pound - obesity I and II
1.6 to 2.0 mcg / pound - obesity III
(Until 2024-09-13 I had
incorrect values here. I gave the mcg / pound figures as mcg /
kg, and did not have mcg / pound figures.)
BMI means Body Mass Index, which can be used as a crude measure of
obesity. See the Wikipedia page
en.wikipedia.org/wiki/Body_mass_index for a chart which looks
up the BMI according to body weight and height. The BMI
formula only applies to adults. It tends to overestimate BMI and so obesity for taller people and
underestimate it for shorter people.
Vitamin D3 quantities are often measured in IUs ("International Units")
which, for vitamin D3 means 1/40,000,000 of a gram. Even though
the quantities are quite small, the numbers of IUs per day can be in
the thousands or tens of thousands.
To convert from IUs to micrograms (millionths of a gram, "mcg" in
medicine, otherwise µg), divide by 40. To convert from IUs to
milligrams, divide by 40,000.
People with
underweight, normal weight and overweight body types should use the first range of ratios:
70 to 90 IU / kg body weight per day vitamin D3
For instance, for 70 kg (154 pounds) this is 4900 to 6300 IUs per day, on average.
5000 IU is 125 micograms = 0.125 mg = 1/8 milligram. This is
a gram every 22 years. (Credit cards weigh about 5.2 grams.)
This could be achieved in several ways, such as:
- One 5000 IU (125 microgram) capsule or tablet a day. Adding
One 1000 IU vitamin D and 200 microgram vitamin K2 MK-7 capsule per day
would be fine too - and vitamin K2 strengthens bones and the immune
system. (In mid-2024 my wife and I take one of these 5000 IU vitamin D capsules a day: www.lifeextension.com/v...0/vitamins-d-and-k-with-sea-iodine
These also provide iodine and three types of vitamin K.)
- One 10,000 IU (250 microgram, 0.25 milligram) capsule 4 times a
week, such as Monday, Wednesday, Friday and Saturday. This is
40,000 / 7 = 5714 IU / day.
- One 50,000 IU (1.25 mg) capsule every 10 days, such as the 10th, 20th and 30th of every month.
People suffering from
obesity I or II should use:
100 to 130 IU / kg body weight per day vitamin D3
As an example, for 110 kg (242 pounds), Prof. Wimalawansa recommends
11,000 to 13,200 IU per day. This could be achieved by:
- One 50,000 IU capsule every 4 days, such as days of the month: 4,
8, 12 etc. to 28. Over a year, this is 11,500 IU a day on average.
- Two 50,000 IU capsules a week for the first three weeks of each
month, and one a week for the rest. This is 88 capsules a year =
12,046 IUs per day on average.
- Two 10,000 IU capsules on Monday and one each day for the rest of the week. This is 11,428 IU per day on average
These ratios are general guidance, not rigid rules. For instance,
for a person whose BMI is 28 , being close to 30, could aim for midway
between the two above sets of ratios, such as for 80 to 110 IU / kg per
day. It is important to find a pattern of taking the capsules
which is easy to remember.
Here is a chart depicting the first two ranges of ratios.
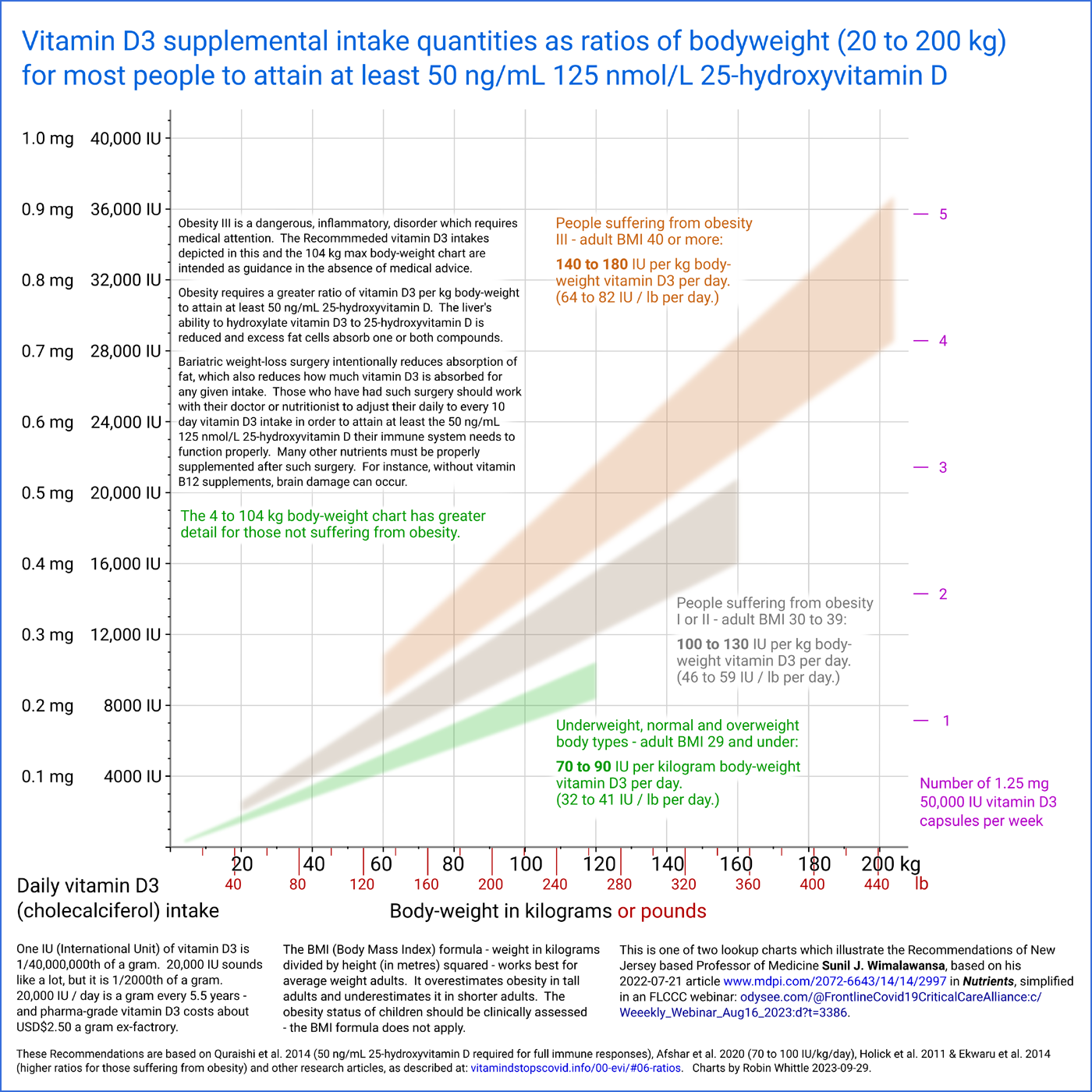
Those suffering from obesity III should seek medical attention for this
debilitating and potentially deadly condition. People who are
unsure whether their obesity would be classified as type II or type III
should aim for an intermediate range or ratios, such as 120 to
160 IU / day per kg body weight.
The top quadrilateral in the following chart depicts the ranges of
ratios Prof. Wimalawansa recommends for those suffering from obesity
III:
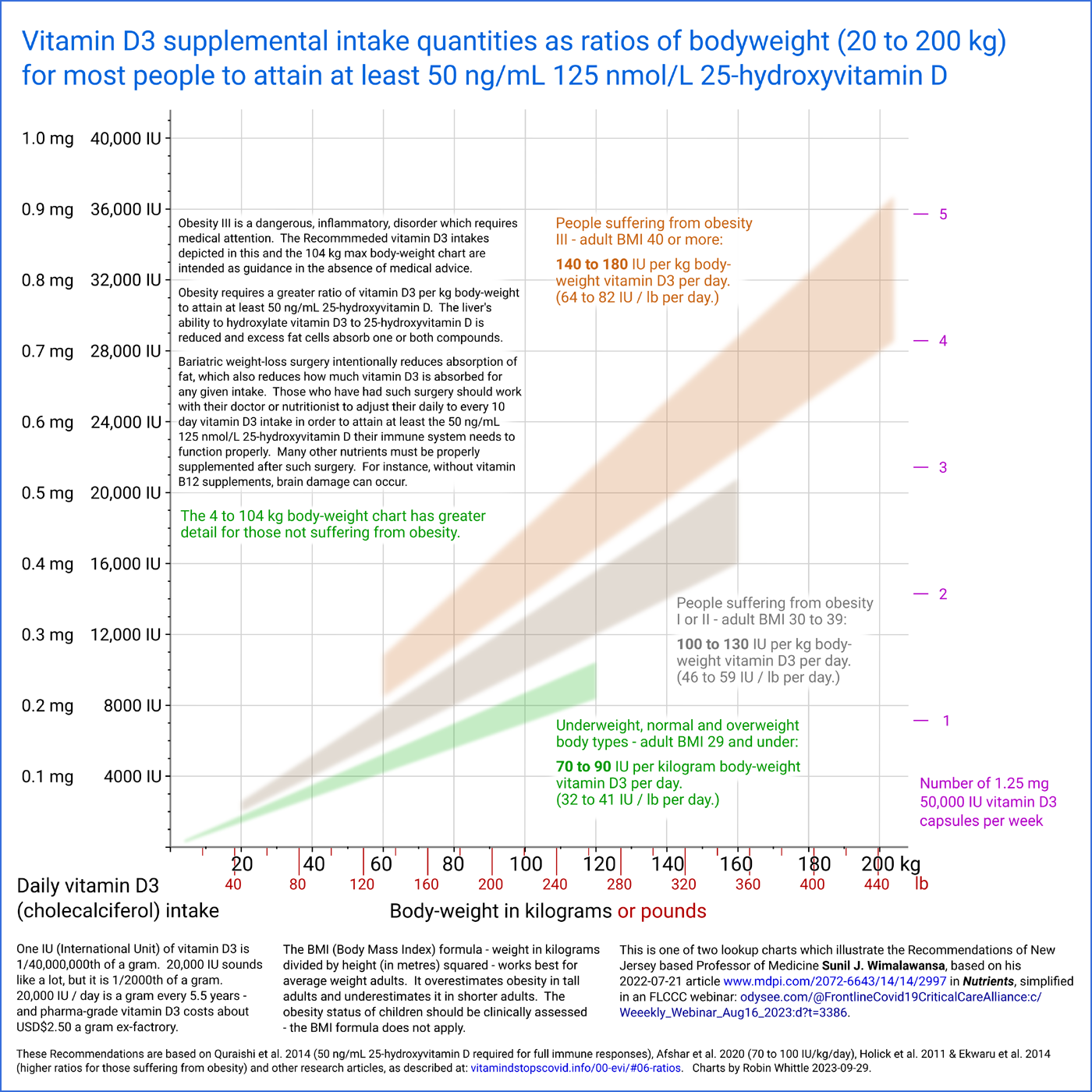
These Recommendations are intended to enable the great majority of people to attain, over several months,
at
least the 50 ng/mL (125 nmol/L) level of circulating 25-hydroxyvitamin
D which their immune system needs to function properly, with no risk of
toxicity. See
#00-50ngmL below.
I will write an article at
nutritionmatters.substack.com about good sources of 1.25 mg 50,000 IU vitamin D3 capsules, such as
www.microingredients.com/products/vitamin-d3-softgel
- 240 capsules for USD$24.95, plus shipping. I ordered some via
Amazon for delivery here in Australia, for AUD$55. For a 70 kg
154 lb adult, 5000 IU vitamin D3 is a good intake, so this is one
capsule every 10 days. At this rate a packet would last 6.57
years = USD$3.80 per year ex shipping and tax.
Please see the section below
#06-ratios on how
these ratios reflect the judgment of Prof. Wimalawansa, based on
decades of clinical and research experience. Prior research indicates
that they are extremely unlikely to cause anyone to attain more than
150 ng/mL (375 nmol/L) circulating 25-hydroxyvitamin D, which as noted
in
#06-ratios:
Although it is not known what the
safe upper value for 25-hydroxyvitamin D is for avoiding hypercalcemia,
most studies in children and adults have suggested that the blood
levels need to be above 150 ng/mL (375 nmol/L) before there is any
concern.
#adv
As far as I know, this is all good guidance on the likelihood of ill
effects resulting from the above recommendations. However, here
is a note on potential problems which are not covered in the
peer-reviewed literature:
Two friends of mine, both in their 60s,
have reported heart arrhythmias (high or erratic heart rates for no
good reason) which they believe were caused by vitamin D3
supplementation in quantities much the same as recommended above.
The second report, with the symptoms appearing at night, seems credible
to me, since the symptoms disappeared within a few days of my friend
stopping his daily 5000 IU vitamin D3 intake, and reappeared within a
day or two of him restarting. He does not use caffeine.
I will write more on this when I have researched it further and
consulted with some vitamin D3 researchers/clinicians. If you
have any such problems, it would be best to stop whatever
supplementation you think might be causing them. Please let me
know about any ill-effects which you think might result from vitamin D3
supplementation: rw@firstpr.com.au . Perhaps there is a pattern
of some people having such ill effects which has so far not been
properly recognised by researchers.
I found two non-peer-reviewed reports which seem to match my friends' experiences:
There is a 2011 conference presentation, which while not peer reviewed,
is the product of formal research with a large number of subjects:
"Abstract 14699: Vitamin D Excess Is Significantly Associated with Risk
of Atrial Fibrillation" Megan B. Smith et al.
www.ahajournals.org/doi/abs/10.1161/circ.124.suppl_21.A14699.
So far, my limited research turned up only one peer-reviewed article
regarding vitamin D and atrial fibrillation: Liu et al. 2019:
nutrition.biomedcentral.com/articles/10.1186/s12937-019-0485-8 . This reports that higher 25-hydroxyvitamin D levels (as would result from vitamin D3 supplementation)
decreased the risk of atrial fibrillation.
Both things may be true: Generally healthy supplemental vitamin D3
quantities, such as those recommended above, which are significantly
greater than those recommended by governments, may reduce the risk of
atrial fibrillation, which is a common and potentially serious form of
heart arrhythmia, in the general population, but nonetheless, in some
individuals, increase the risk.
#sjw-article
Please see
Prof. Wimalawansa's July 2022 article, in the prestigious journal
Nutrients:
Rapidly Increasing Serum
25(OH)D Boosts the Immune System, against Infections - Sepsis
and COVID-19
Sunil J.
Wimalawansa (See:
#10-sjw-bio for an account of his decades of research on vitamin D.)
Nutrients
2022-07-21
www.mdpi.com/2072-6643/14/14/2997
In addition to the earlier, more
complex, version of the above recommendations for vitamin D3
supplemental intake as ratios of body weight, this article also
discusses the use of a
single oral dose of 0.014 milligrams of calcifediol
per kg body weight, to raise circulating 25-hydroxyvitamin D levels
safely over
50 ng/mL (125 nmol/L) in 4 hours. See:
#4.7 and
https://nutritionmatters.substack.com/p/calcifediol-to-boost-25-hydroxyvitamin . This is about 1 milligram for 70 kg. Calcifediol
is
25-hydroxyvitamin D. If this is not available, a single oral bolus
dose of ca. 10 mg 400,000 IU vitamin D3 cholecalciferol should be used (for 70 kg body weight),
but this takes about 4 days due to the need for hydroxylation in the
liver.
This is the most important step to take, as early as possible,
in almost any condition which
constitutes a
clinical emergency,
especially sepsis, COVID-19, ARDS, Kawasaki disease etc. for the vast
majority of the population who have not been supplementing vitamin D3,
for months, in sufficient quantities to attain
50 ng/mL.
Prof. Wimalawansa's article draws a strong distinction between how 1,25-dihydroxyvitamin D (calcitriol) is used in
hormonal signaling - by which the kidneys regulate calcium-phosphate-bone metabolism throughout the body - and the lesser known
intracrine and paracrine signaling
(as described below:
#02-compounds) systems used by many types of cells, especially immune cells.
He uses the term "autocrine" signaling for what is actually vitamin D based intracrine signaling.
(Intracrine means the receptor is in the cytosol while autocrine means it is on the outside of the cell's membrane. I made the same mistake.)
Most doctors and immunologists are not familiar with 25-hydroxyvitamin D based
intracrine or paracrine signaling. If they think of vitamin D and the
immune system at all, (many don't) they tend to assume that the circulating,
hormonal (endocrine signaling) level of 1-25-dihydroxyvitamin D somehow
"regulates" or otherwise affects immune cells. It does not, as Prof.
Wimalawansa explains and as I do in section
#02-compounds below.
The widely believed statement that "vitamin D is a hormone" is dangerously misleading
since it leads people to be overly-cautious
about supplementing vitamin D3 cholecalciferol. It also leads to
treatment decisions in clinical emergencies which are firstly of no
help to the immune system and secondly which are likely to disrupt
calcium-phosphate-bone metabolism: raising circulating
1,25-dihydroxyvitamin D levels, such as by oral or injected/IV
calcitriol. There is no need to alter this level. The immune
system needs
25-hydroxyvitamin D.
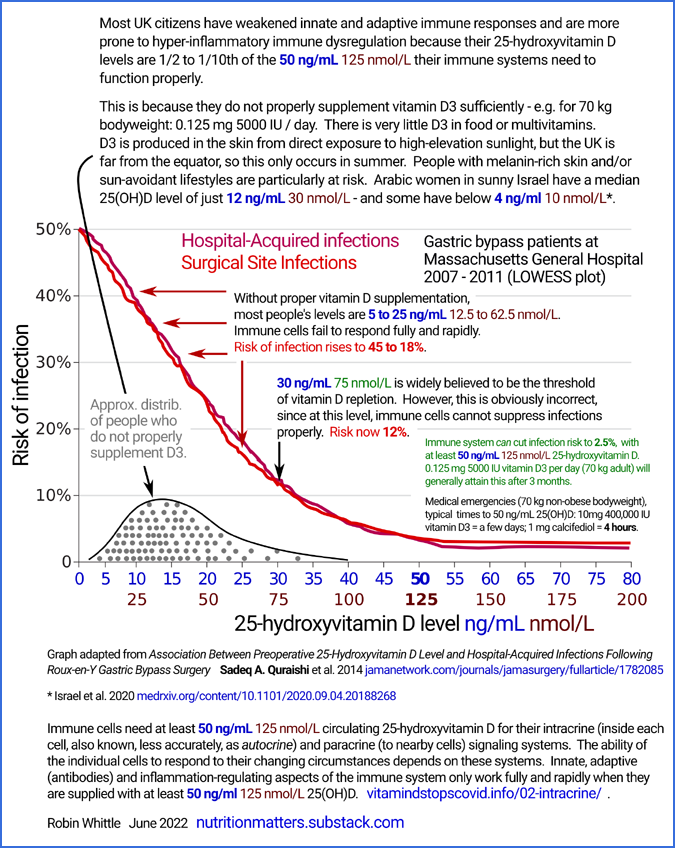
#00-quraishi #00-50ngmL
00 At least 50 ng/mL (125 nmol/L) circulating 25-hydroxyvitamin D is needed for proper immune function
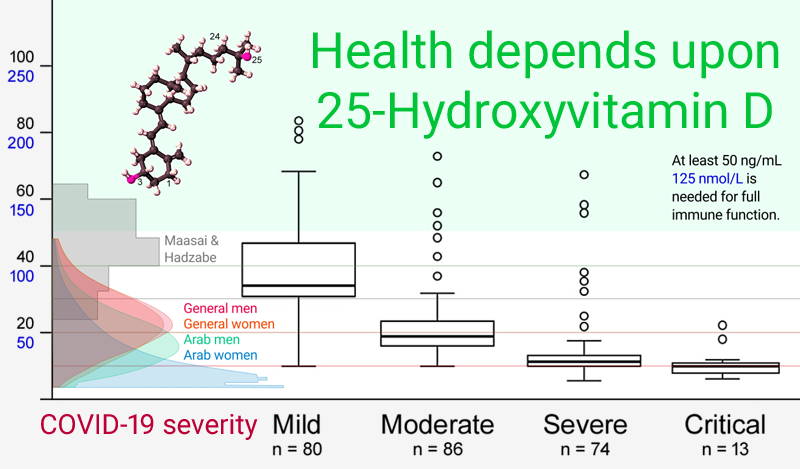
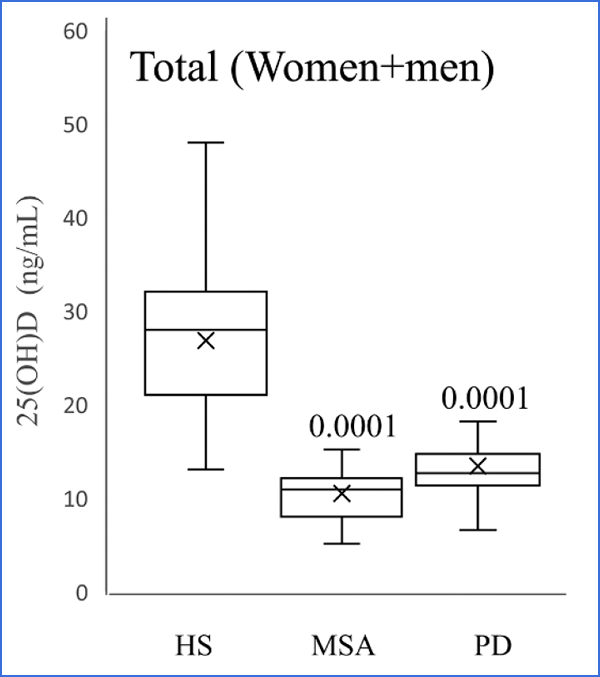
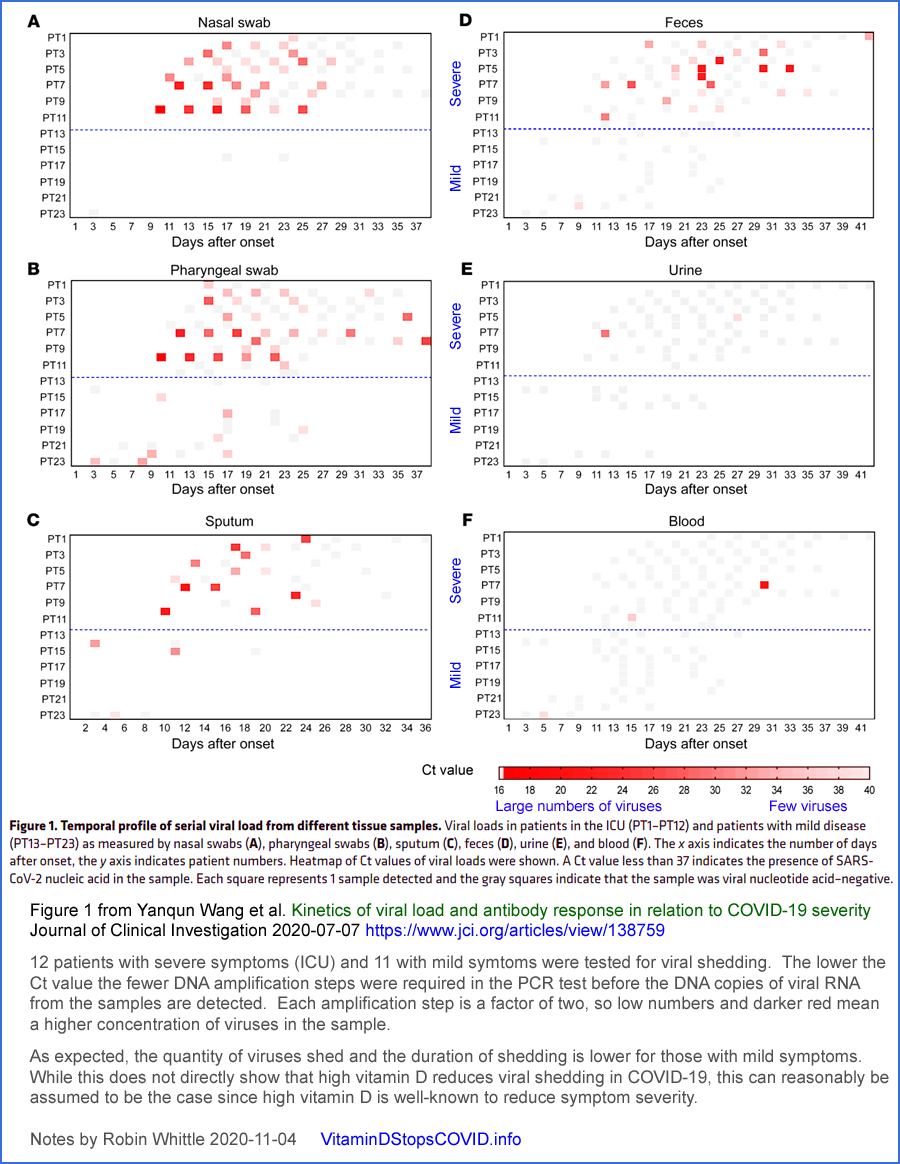
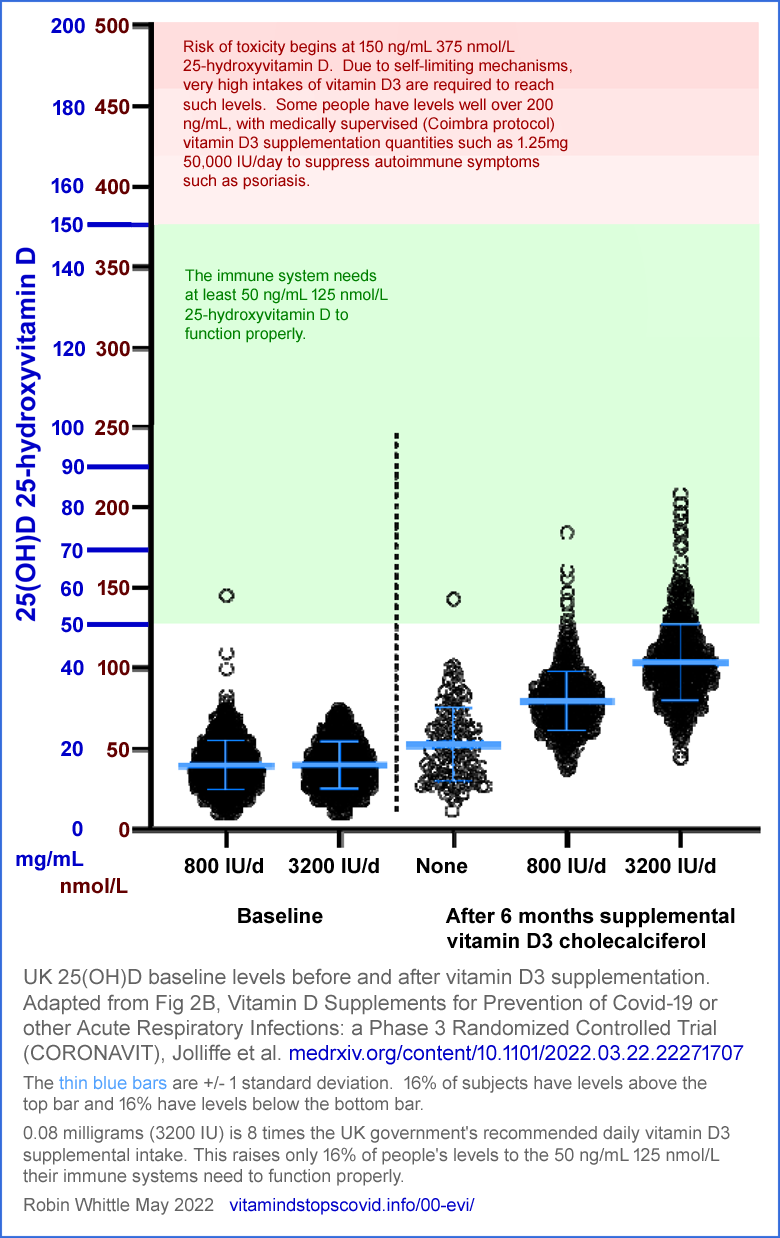
The above graph is adapted from the two graphs at:
These two similar graphs - which depict low pre-operative 25-hydroxyvitamin D levels causing immune system failure,
which leads to greatly elevated risk of post-operative infections - are from arguably the most important
and easy-to-understand research study on the importance of good
25-hydroxyvitamin D levels for the immune system.
This is from Massachusetts General Hospital, showing the risk of primarily bacterial
infections rises strongly from about 2.5% (for both
hospital-acquired and surgical-site infections) according to how far
below 50 ng/mL (125 nmol/L) their pre-operative level of
25-hydroxyvitamin D was.
The risk of each type of infection multiplies by a factor of 5 to
about 25% when levels
are 20 ng/mL (50 nmol/L). This is the official threshold of
vitamin D sufficiency in the UK.
Many UK adults and children have still lower levels, such as 5 to 10 ng/mL (12.5 to 25 nmol/L),
and so, for all their lives, are at great risk of suffering and harm,
due to their immune systems being unable to function anywhere near as
well as they would with proper vitamin D3 supplementation.
The 770 patients in this study were all morbidly obese and underwent the
same Roux-en-Y gastric bypass operation, which is a complex
surgery intended to help with weight loss. There is no reason to believe that people suffering from
obesity require higher 25-hydroxyvitamin D levels for proper immune
system function than do those who are not suffering from obesity.
So we can reasonably assume that this stark relationship between immune
system efficiency and 25-hydroxyvitamin D level, applies to most people
in general.
#01-intro
1 Introduction
1.1 Key points
This
Call for evidence
is most welcome. One of the world's leading vitamin D
researchers, Professor Martin Hewison (
University of Birmingham),
stated that "
England
is the centre of vitamin D deficiency" and that rickets is still found in
some communities in pediatric clinics all over the UK.. This is
in a March 2021 interview youtu.be/QjbZFupJsMY?t=457 in which one of his slides was:
Scotland has even lower
average levels of circulating 25-hydroxyvitamin D and all over the
country, those with dark skin, sun-avoidant lifestyles, the elderly and
those suffering from obesity are even more likely to have disastrously
low vitamin D levels.
The research articles cited below show beyond doubt that:
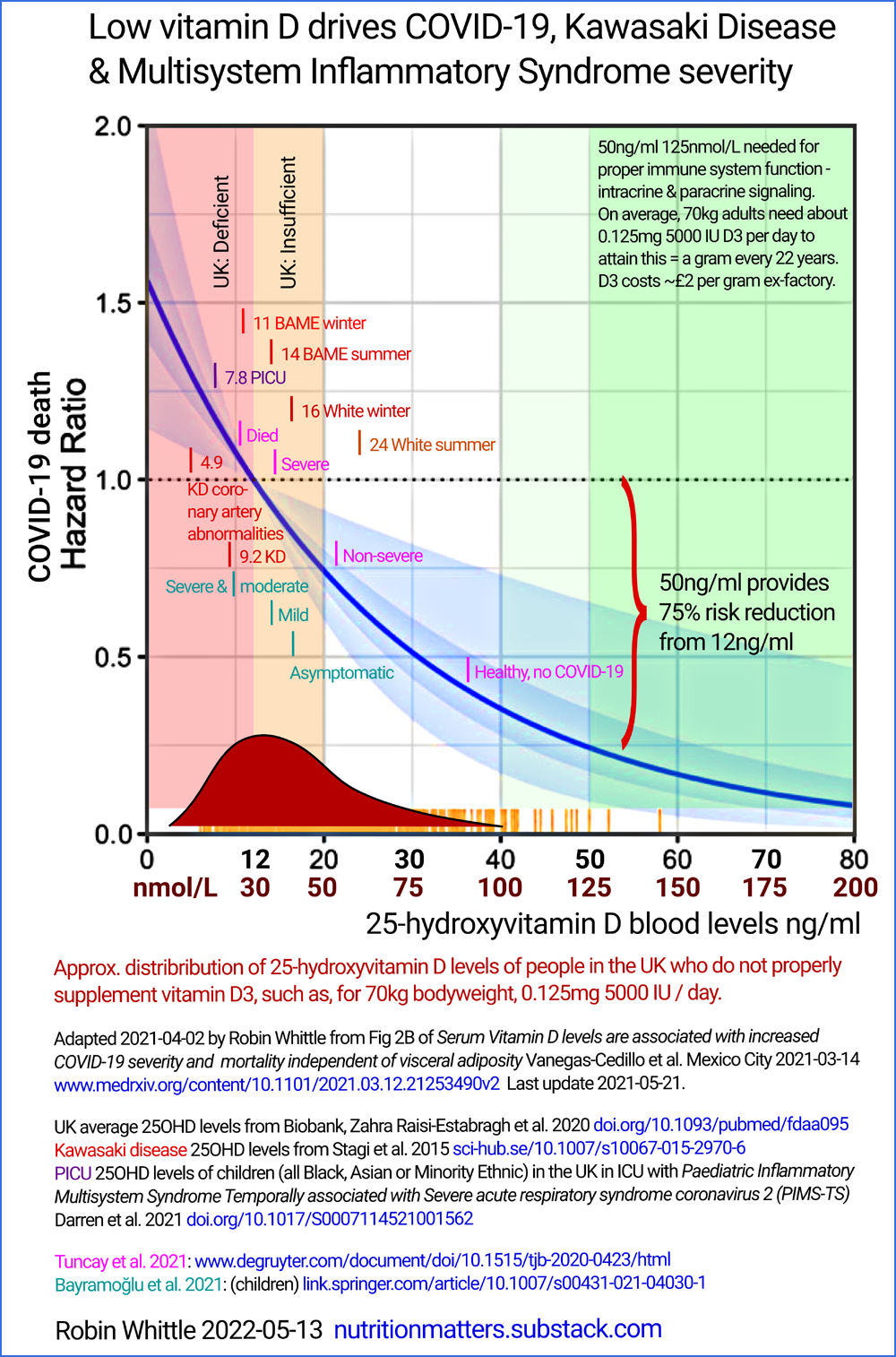
- 50 ng/mL (125 nmol/L) circulating 25-hydroxyvitamin D (25(OH)D) is the
proper standard of vitamin D repletion, because levels below this cause
weakened innate and adaptive immune responses and raise the risks of
self-destructive, hyper-inflammatory (cell destroying) immune responses. [Quraishi et al. 2014 above and #50ngml.]
- The current standard of vitamin D sufficiency in the UK - 20 ng/mL (50 nmol/L) 25(OH)D is 60% too low.
The
UK's 25(OH)D standard of repletion is based on 2011 decisions by the
North
American Institute of Medicine (IOM) which were challenged at the time
by knowledgeable researchers, regarding the needs of the immune
system. The IOM's deliberations were based solely on the
needs of the
kidney to regulate calcium-phosphate-bone metabolism.
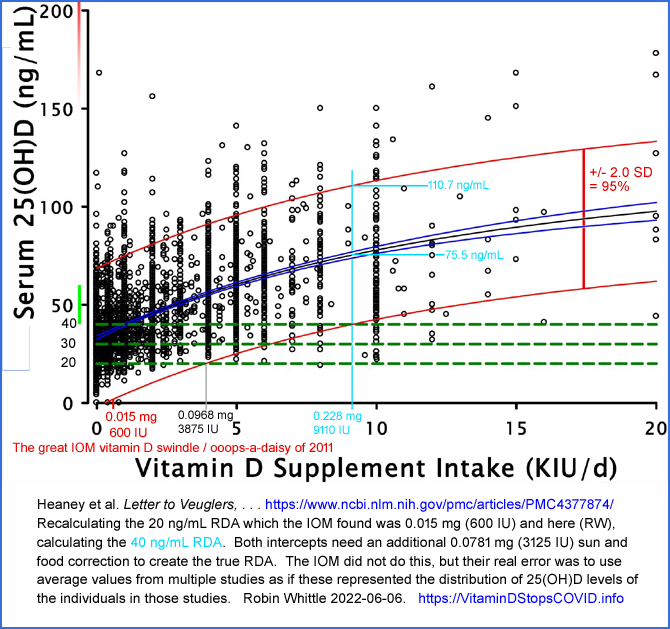
The IOM's statistical method for determining the RDA (Recommended Daily
Allowance) of vitamin D3 was shown, several years later, to be entirely
mistaken. In order to determine the amount required to attain at
least a 20 ng/mL (50 nmol/L) 25(OH)D level in 97.5% of the adult
population, they used the variance of the averages of several trials,
when they should have used the variance of all the individuals in those
trials. They calculated an RDA of 0.015 mg 600 IU.
Subsequent calculations using the studies chosen by the IOM showed the
real RDA for this 25(OH)D level is about 0.175 mg 7000 IU.
However, the IOM report has never been amended, and remains to this day
the foundation of the guidance most or all governments provide for
their citizens. [#05-history.]
Due in part to the great variation in body-weight between adults, an
RDA
is impractical for vitamin D. The only reliable way of attaining
good 25(OH)D levels for all people from birth to old age, with all
their variation in body-weight and obesity, is to specify vitamin D
supplemental intake quantity as a ratio, or range of ratios of
body-weight, with higher ratios for those suffering from obesity.
Vitamin D can be taken weekly or every 10 days. There is no need
to take it every day, since the half-life of 25(OH)D is a month or
so. [#06-ratios and #00-how-much]
- In
general, a person who is not suffering from obesity, with a body-weight
of 70 kg, requires 0.125 mg (5000 IU) to 0.175 mg (7000 IU)
vitamin D3 a day to maintain 50 ng/mL (125 nmol/L) or more circulating
25-hydroxyvitamin D. [#06-ratios.]
The current UK recommendation for adults of 0.01mg (400 IU)
supplemental vitamin D3 per day is less than a tenth of what a 70 kg
non-obese person needs to maintain proper immune system function. [#05-history.]
- The health benefits of proper supplementation, for all people
other than infants being substantially breast fed by vitamin D replete
mothers, are profound and far-reaching.
- Since there is little vitamin D3 in food (fortified or not) and
in multivitamins - and since UV-B skin exposure is not always available
and always damages DNA and so raises the risk of skin cancer - daily to
weekly (or three times a month) supplementation is the only way most people can attain proper
25-hydroxyvitamin D levels all year round.
Fortunately, the quantities required are small. 5000 IU/day is a
gram every 22 years, and ex-factory, pharmaceutical-grade vitamin D3 costs ca. £2 (USD$2.50) a gram in
1 kg lots.
These supplementation levels are well researched and far below the intakes which might lead to toxicity.
- Food fortification with vitamin D has numerous problems. No
practical consumption levels of fortified food can provide more than a
small fraction of the vitamin D each person needs to attain 50 ng/mL (125 nmol/L)
25-hydroxyvitamin D sufficiency. So it would be dishonest to
support or promote this as government policy.
All efforts and resources which might be considered to introduce or
expand vitamin D food fortification would be better dedicated to
education and support for proper daily to weekly (or the 10th, 20th and 30th day of each month) vitamin D3
supplementation. [#07-fortif.]
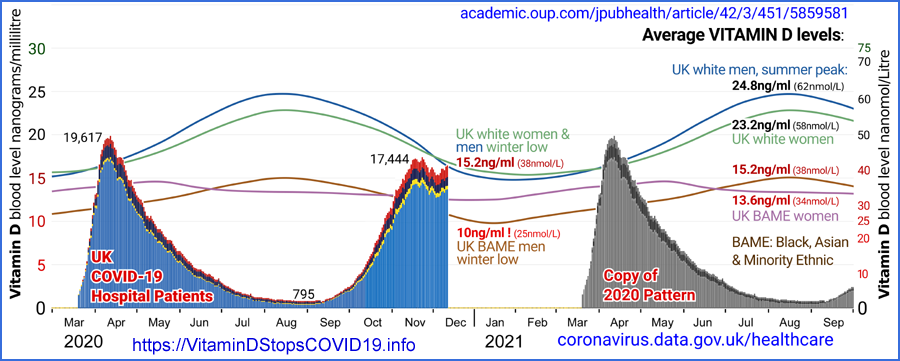
1.2 This website's name
The name of this site
vitamindstopscovid.info
was chosen in late 2020 based on two principles. While high 25-hydroxyvitamin D levels
may somewhat reduce the chance of contracting COVID-19, for any given
viral insult, good (50 ng/mL 125 nmol/L or more) levels
stop (at least with the variant of mid-2020 in the UK)
pandemic transmission by
greatly reducing the severity of illness and so reducing the average
rate of viral shedding to below that required for pandemic transmission,
even in the absence of lockdowns or COVID-19 vaccines. Evidence
for this is presented below
#4.2.
#04-health
While this is not provably the case with current variants, the
transmission and severity of all COVID-19 variants can best be reduced
by ensuring that as many people as possible have at least 50 ng/mL (125
nmol/L) 25-hydroxyvitamin D levels AND that they are provided with
multiple
early treatments, the most effective of which are much safer, more
effective and less expensive than the patented, highly profitable,
treatments (vaccines included) which are promoted by
multinational pharmaceutical companies.
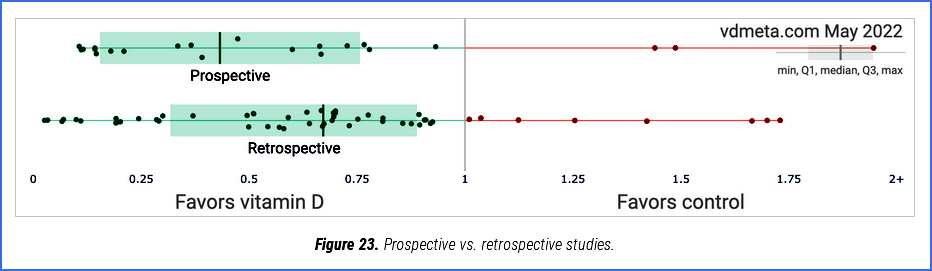
There are numerous observational studies showing COVID-19 severity
correlating with low 25-hydroxyvitamin D levels. These low
levels are common in the UK, and almost ubiquitous in people with dark
skin and/or sun avoidant lifestyles who do not properly supplement
vitamin D.
The disastrous suffering, harm, death and social and economic
disruption of the COVID-19 pandemic could have been rapidly halted
in 2020 if all governments had worked assiduously to ensure their
populations had sufficient vitamin D3 for their immune systems to work
properly.
Yet the real harm, death, cost and disruption of sub-125 nmol/L 25
hydroxyvitamin D levels is much greater than that caused by COVID-19. It
includes sepsis, dozens of inflammatory autoimmune disorders, cancer, Kawasaki
disease, MIS-C and acute complications, pre-term birth and lasting
developmental disorders of pregnancy. Sepsis alone kills 11 million people a year, worldwide:
www.thelancet.com/journals/lancet/article/PIIS0140-6736(19)32989-7.
1.3 Author's background
Although I have lived in Australia since 1961, I am a British citizen
by virtue of being born in Wantage (1955). I work with computer
programming and electronic musical instruments. Like many other
technically-minded people with no medical training, I became involved
in raising awareness of vitamin D's importance to the immune system
some years ago, once I realised that this gross and easily-correctable
deficiency afflicts the great majority of the world's population.
In July 2020 I established the Nutrition for Immune System Health (NISH) email discussion list:
nish.groups.io
. Members include some of the world's leading vitamin D
researchers. I collaborate with some of them in raising awareness of the importance of vitamin D, such as with this
submission.
I have no qualifications or expertise regarding medicine or nutrition. Please
do not take my word for anything. My purpose in writing is to
prompt a full awareness of the most pertinent research articles.
Please read these articles!
1.4 Most doctors do not understand vitamin D's importance to the immune system
The question of why many or most doctors, immunologists,
virologists, epidemiologists and public health officials are not
properly aware of vitamin D's importance to the immune system is a vast
and perplexing topic, beyond the scope of this submission.
However, some key points should be recognised:
- These people are very busy dealing with myriad complexities and threats to health.
- Doctors in particular are overloaded with information and
responsibilities - and much of this information arises from
pharmaceutical companies trying to convince the doctor to prescribe
their most expensive, profitable, products. This includes the
pernicious influence of these companies on the revenues and policies of
academic journals, and on the selection and views expressed by the
members of government advisory committees.
Unlike the
pharmaceutical industry, vitamin D researchers are academics and/or practicing doctors and nurses who do not belong
to an industrial bloc seeking to sell a product, at a profit, to governments
and the medical establishment. They do
not have an economic agenda, let alone the funding to promote one.
- The vitamin D research literature is sprawling and it can be difficult to locate the most pertinent research.
- No
journal article properly explains - to those who do not already
understand it - how 25-hydroxyvitamin D is used by multiple types of
immune cells for their intracrine (AKA, less correctly, autocrine) internal signaling systems and their related paracrine
signaling to nearby cells. This is unrelated to the hormonal
model of vitamin D metabolism with the kidneys regulating
calcium-phosphate-bone metabolism.
The immune system is second only in complexity to the nervous
system. Coordination between its individual cells of multiple
types relies on numerous signaling molecules, such as cytokines [WP <<< Wikipedia link for general background information], and
also to some extent on vitamin D based paracrine signaling.
The
ability of individual immune cells to respond to their changing
circumstances is highly dependent on 25-hydroxyvitamin D based intracrine
signaling.
The details differ from one cell type to the next, but the
common principle is that this signaling system enables a cell to
respond to a particular condition by rapidly changing its gene
expression and so the behaviour of the whole cell. This powerful,
intracellular, signaling capability is the way most cell types use
25-hydroxyvitamin D. The kidney-based hormonal use of
25-hydroxyvitamin D, which it converts into a very low level of
circulating
1,25-dihydroxyvitamin D for hormonally regulating calcium-phosphate-bone
metabolism is very well known, but is only one of dozens of functions
of
the vitamin D compounds.
A proper understanding of vitamin D based intracrine and paracrine
signaling is far beyond the knowledge of most doctors, immunologists,
etc. - and even beyond the knowledge of many people who research
vitamin D. My first tutorial on these signaling
systems is: vitamindstopscovid.info/02-intracrine/ . I wrote this because I found no journal article which introduces the mechanisms in a tutorial fashion.
An understanding of these signaling systems is absolutely essential to
a proper understanding of the importance of good, 50 ng/mL (125 nmol/L) or more
25-hydroxyvitamin D levels for human health. As such, every
doctor, immunologist, virologist, vaccinologist, epidemiologist and
public health official is flying blind if they do not understand the vitamin D based intracrine and paracrine signaling systems and have at least a general grasp of how important
they are. Without proper supplementation, most people today have 1/10 to 1/2 of the circulating 25-hydroxyvitamin D their
immune cells need to function properly.
- Medical
doctors are generally poorly trained in nutrition and have been
regaled with promotion of various nutrients over the years.
Many regard claims such as those made for vitamin D as being too simple
- too good to be true. They may also find it difficult to convince
some of their patients of the importance of nutrition.
They should read the most pertinent research, as cited and discussed here.
A growing proportion of the population is aware of the need for much
improved vitamin D supplemental intakes to enable the immune system to
work properly. Still, many doctors - while able to do extraordinary
work in many difficult, complex,
situations - are insufficiently aware of the nutritional deficits and
imbalances which worsen or cause numerous chronic and acute diseases,
the most prominent of which is vitamin D3.
- A
patented compound even a fraction as effective as vitamin D3 would be
enormously profitable and so very strongly promoted. Vitamin D3
cannot be patented. There is very little money to be made from
it. None of the major pharmaceutical companies make or resell
vitamin D3 cholecalciferol. So for-profit pharmaceutical companies
benefit from promoting
their expensive, complex, supposedly sophisticated products - the need
for which would be greatly reduced if most people had sufficient
25-hydroxyvitamin D for their immune systems to work properly.
See long-time vitamin D researcher Bill Grant, PhD's 2018 account of the
hostile, unprincipled, actions of some multinational pharmaceutical
companies regarding vitamin D: Vitamin D acceptance delayed by Big Pharma following the Disinformation Playbook http://orthomolecular.org/resources/omns/v14n22.shtml.
- The
core principles of vitamin D and the immune system are not
particularly complex. They are different from the hormonal model all
doctors are fully familiar with, which applies only to the role of the
kidneys in regulating calcium-phosphate-bone metabolism. There
has been a greatly
regrettable tendency to think of vitamin D (collectively vitamin D3
cholecalciferol, 25-hydroxyvitamin D calcifediol and
1,25-dihydroxyvitamin D calcitriol) as "hormones". This has led
to unrealistic concerns about toxicity resulting from
supplementation. Calcitriol is the only one of these compounds
which acts as a hormone - when it is produced by the kidneys, and
circulates at a very low level in the bloodstream for signaling to
multiple cell types all over the body, to
regulate calcium-phosphate-bone metabolism.
Immune cells' production of calcitriol is unrelated to hormonal
(endocrine) signaling. In and between these cells, it acts as an
intracrine agent or a paracrine agent, at a much higher concentration
than the kidneys' hormonal calcitriol. This intracellular
production of calcitriol does not affect
calcium-phosphate-bone metabolism.
- Many concerns about vitamin D toxicity are not founded on the best research.
There is a strong self-limiting mechanism for 25(OH)D which means that
the range of vitamin D3 intakes which provide a healthy range of
25(OH)D levels is very wide. This is not the case for vitamin A,
iron and many other nutrients.
With body-weight ratio based supplemental vitamin D3 intake quantities,
it is both practical and desirable for all people to maintain good
25(OH)D levels without the need for testing or medical involvement.
1.5 Action based on evidence, rather than on the mistaken views of many doctors, immunologists, etc.
The
Secretary of State for Health and Social Care has asked the newly
established OHID to solicit evidence from the public regarding
improvements to the vitamin D status of people in England.
There's only so much which can be done within the current misguided
and
ill-informed existing recommendations. All the research mentioned
below indicates that the vitamin D guidance by the UK or at least
English government is completely inadequate to the task of maximising
health.
Other UK government health organisations have declined to alter their
extraordinarily low vitamin D intake recommendations and associated
target 25-hydroxyvitamin D levels. Asking them to review the
evidence would mean they would have to admit they were wrong in the
past, if they were to revise their guidance to suit people's real needs.
Below you
will find
observational and experimental evidence
and some well-informed clinical and research opinions/judgments
which show that current government guidance and the understanding of
most medical doctors is way out of date, and needs to be revised in
order that most people, naturally and normally, have sufficient
circulating 25-hydroxyvitamin D for their immune systems to function
properly. When they do, their kidneys will have no difficulty
maintaining the much lower level of circulating 1,25-dihydroxyvitamin
D calcitriol, which hormonally regulates calcium, phosphate and bone metabolism.
Those not directly involved in nutrition and medicine reasonably assume
that most doctors - and especially specialist researchers such as
immunologists - keep up to date on the latest research which is
pertinent to their many concerns. This is generally not the
case with vitamin D. The failing is partly due to vitamin D
researchers not clearly explaining the intracrine and paracrine
signaling systems of immune cells, which only operate properly with 125
nmol/L or more circulating 25-hydroxyvitamin D. Some other causes
of this disastrous lack of understanding are listed above.
Given that multiple types of immune cell rely on these 25-hydroxyvitamin D
based signaling systems in order that each cell can respond properly to
its changing circumstances, one might think that immunologists would be
interested in this and generally up to speed. However, this is
not the case. Research fields can be like silos, or ships passing
in the night, with their inhabitants already busy with numerous
detailed and urgent concerns.
I recently bought two of the best regarded immunology texts:
Janeway's 9th 2016 and
' 10th 2021, comprising 1500 pages of beautifully illustrated and fascinating
detail. "Vitamin D" does not appear in either book's index.
Your responsibility is to the people of the UK and more broadly of all other countries (whose government guidance and medical
knowledge are not much better than those in the UK). Please
evaluate the evidence on its merits.
By developing new, fully research-based, official recommendations, you
can set new standards for government guidance and support for doctors'
proper understanding of vitamin D. By doing so you can right past
wrongs, lead England and the UK from its currently widely recognised
(among vitamin D MDs/researchers) status as one of the worst nations on
Earth for vitamin D, to leading the world in this regard. There's
no space to detail the history of vitamin D here, but Britain played
the leading role in research and standardisation, beginning in the
1920s.
By the way, it is common for people in the UK to pronounce the first
syllable of "vitamin" in a weak, almost apologetic, manner: to rhyme
with "bitter". Please follow the lead of most other English
speaking people,
and
Professor Martin Hewison, by pronouncing this word with the oomph it
deserves, to rhyme with "vital", since it was derived from the Latin
"vita".
#02-compounds
2 The three vitamin D compounds, and the history of units for these
and for 25-hydroxyvitamin D levels; vitamin D based intracrine and
paracrine signaling
Almost all of what is currently
reliably known about "vitamin D", the immune system and
calcium-phosphate-bone metabolism is based on the three compounds
described below.
Vitamin D2 ergocalciferol is a similar molecule to the naturally
occurring (in mammals) vitamin D3 cholecalciferol. There are
25-hydroxy and 1,25-hydroxy forms of vitamin D2, but all three
compounds are less functional and so less helpful at maintaining health
than their vitamin D3 based equivalents. Please see:
Jones et al. 2014 and
Hicks 2022.
For obscure historical reasons, doctors in the USA often prescribe
vitamin D2,
which is made from yeast, while vitamin D3 is usually made from 7-dehydrocholesterol
derived from wool fat. Since there are vegan sources of vitamin D3, there
are no reasons for using vitamin D2 and it will not be mentioned
further below.
The terms "vitamin D" or "vitamin D3" are often used collectively
to refer to the three compounds mentioned next. A common failing in
the research literature is to use "vitamin D" when the author is
referring to a specific compound which should be clearly
identified. This was pointed out in 2004:
Only the first of these three compounds is a vitamin. Only the
third of these compounds can function as a hormone - for
calcium-phosphate-bone metabolism. The many immune system
functions of the vitamin D compounds do not involve hormonal signaling.
Vitamin D's first-recognised function (regulating
calcium-phosphate-bone metabolism) put the compounds within
the field of endocrinology (hormonal signaling), yet their immune system functions
fall within immunology, not endocrinology.
2.1 Vitamin D3 cholecalciferol
For brevity, I will generally refer to this below as
D3.
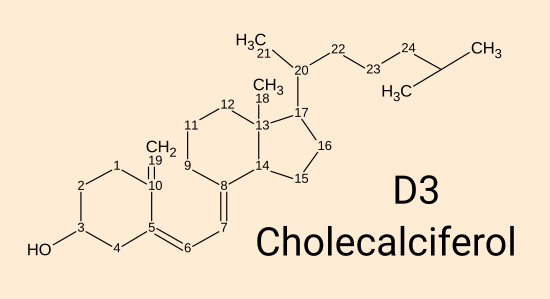
D3 cholecalciferol. [
WP] is produced by the approximately 295 to 297 nanometre
wavelength range of UV-B light acting on 7-dehydrocholesterol in the
skin. It can also be ingested in food or supplements. While
this plain D3 directly
protects the endothelial cells which line our blood vessels [
Gibson et al. 2015],
all its other currently known roles in the body rely on it being
converted primarily in the liver (there may also be some conversion in
cells outside the liver), over a period of days to a week, by the
enzyme vitamin D 25-hydroxylase (encoded by the
CYP2R1
gene, a name sometimes given to the enzyme itself) to the second compound 25-hydroxyvitamin D AKA 25(OH)D.
(Another enzyme encoded by the CYP27A1 gene does the same thing and so
produces some of the 25(OH)D.)
The numbers indicate carbon positions. Most hydrogen atoms are
not shown.
In Nature, in the laboratory and in industry, the only method by which this or
similar molecules can be produced is by starting with a molecule with
four carbon rings, and then by breaking the double-bond between carbons
9 and 10, to open up the second ring. No chemical reaction can do
this. The only way of breaking the bond is with the energy imparted to particular electrons by 295 to 297 nanometre
UV-B light.
Ultraviolet-A light - 315 to 400 nanometre
wavelength - is shorter wavelength (higher frequency, higher
energy induced in electrons) than visible violet. The light which creates D3 falls within the UV-B
band, 280 to 315 nm. This is right at the limit of the Sun's
shortest wavelengths and is attenuated both by the ozone layer and the
lower atmosphere. All UV-B light breaks bonds in other biological molecules,
such as DNA, and so damages genetic information in our cells and
predisposes them to cancer.
Industrially, D3 is produced in a handful of highly specialised
factories, with most production being for agricultural animals. The
factories which produce pharma-grade D3 are primarily in India and
Europe. None are in the Americas or the British Isles.
7-dehydrocholesterol, prepared in a series of chemical steps, from wool fat, is dissolved in benzene
and irradiated with specialised multi-kilowatt mercury vapour lamps
which have been doped to produce the requisite wavelengths. A
full account of industrial production of vitamin D3 is
Industrial Aspects of Vitamin D by
Arnold L. Hirsch in 2010 :
sci-hub.se/10.1016/B978-0-12-381978-9.10006-X .
Fermenta Biotech in India is one of the
few companies worldwide who produce pharmaceutical grade vitamin D3
cholecalciferol, though most of their production is for agricultural animals.
None of these vitamin D3 factories are owned by the major multinational
pharmaceutical companies. Industrial production requires a lot of
electricity and is highly competitive. Pharma grade vitamin D3
sells for around USD$2500 per kg, which is just under £2 per
gram. For a 70 kg non-obese person to maintain healthy 50 ng/mL (125
nmol/L) 25(OH)D levels, 0.125 mg (5000 IU) vitamin D is required a day.
This is a gram every 22 years.
Raw vitamin D3 is produced in the same way, and sometimes in the same
factories, for agricultural and human use. The latter is refined more
carefully.
The SI [
WP] units for measuring D3 supplemental intakes are milligrams and micrograms,
mg and
μg respectively, where the Greek lowercase Mu is commonly replaced with lower case
u. In medicine, micrograms are typically denoted as
mcg
in an effort to avoid confusion between the two SI units.
However, the most common unit for specifying vitamin D3 intakes is a
curious unit: the International Unit (IU) [
WP].
The very small mass of this unit, for D3, bedevils the field and
blights human health because ordinary healthy daily intakes involve
thousands, or tens of thousands, of IU. These scarily high
numeric values harm human health by making doctors, regulators and
ordinary people unnecessarily wary about recommending the quantities
which are required for proper health.
The concept of an International Unit applies to only a handful
of nutrients or hormones, and for vitamin D3, one IU specifies 1/40th
of a microgram: 1/40,000,000 gram.
DeLuca 2014
History of the discovery of vitamin D and its active metabolites traces the history of its discovery to concern about the very high prevalence of rickets [
WP]
("The English Disease") in the UK, especially Scotland, ca. 1914.
The molecular structure of 7-dehydrocholesterol and vitamin D3
cholecalciferol was determined in 1937 and until 1968 it was assumed
that this D3 molecule was directly responsible for its health
benefits, known at the time as enabling proper calcium-phosphate-bone
metabolism, specifically by the avoidance of rickets.
The IU for vitamin D arose in the 1920s and 1930s in an international
effort to standardise testing of products which contained vitamin D,
for the urgent purpose of preventing rickets. Vitamin D's chemical
structure was not known and the only way of assaying the vitamin D
content of a substance was to feed various amounts of the substance to
baby rats, who had been fed a special diet which caused them to develop
rickets unless they ingested sufficient vitamin D. These rat
assays remained the only method available for measuring vitamin D until about the 1960s.
Vitamin D3 cholecalciferol is more soluble in fat than in water,
since it only has one hydroxyl
group. (This is on the 3rd carbon. This is unrelated to the
'3' in "vitamin D3".) It is a waxy, semi-crystalline solid at
room temperature. It
is normally sold diluted in tiny "spray dried" granules of hydrogenated
vegetable oil which is solid at room temperature and coated with a
starchy powder to stop the granules sticking together. This is
put into capsules, made into tablets or added to fortified food.
It may also be dissolved in oil.
While levels of D3 can be measured in the blood, this has no clinical
significance, since its primary role is to be hydroxylated, mainly
in the liver, to 25-hydroxyvitamin D. The half-life of vitamin D3
in the bloodstream is in the order of 4 days to a week. Only
about 1/4 of ingested vitamin D3 it is converted into circulating 25(OH)D.
A
vitamin is an organic molecule which
the body needs in small quantities to function properly. Vitamin D3 is
arguably not a vitamin, since in certain environments we can produce all we need ourselves with UV-B
exposure of our skin.
However, for most people, it is impossible to obtain all the vitamin D3
they need from UV-B skin because they cannot expose their skin enough
all year round. Even if this was possible, it would never
be advisable due to the skin damage and cancer risk this would entail
over a
lifetime. (Here in Australia, everyone knows about skin
cancer. Awareness of this is much lower in the UK.) So
vitamin D3 can be properly considered a vitamin.
In mammals, a
hormone is a substance which,
by its level (concentration) in the bloodstream (dissolved in the
plasma, rather than being in the blood cells themselves) signals from
one part of the body (whatever controls this level) to cells in distant
parts of the body, information which controls the distant cells'
behaviour. Hormones may also circulate in the cerebrospinal fluid.
The level of vitamin D3 cholecalciferol in the blood or anywhere else
does not signal anything - meaning it does not convey information from
one part of the body to another.
Vitamin D3 never acts as a hormone.
A common failing of vitamin D research articles is to refer to
vitamin
D3, or the three compounds collectively ("vitamin D"), as a
"hormone". This is
often an attempt to ascribe to it a gravitas it is thought to lack as
a mere "vitamin". This is a mistaken description, except in one
particular instance, as Reinhold Vieth (above) explains. This
common mistake gives rise to unreasonable concerns about vitamin
D3 intakes which might be regarded as ingesting a hormone, and so leads
to unrealistic fears about toxicity.
D3 does not bind strongly to the Vitamin D Receptor (VDR) [
WP]
- the large molecule, which when bound to 1,25-dihydroxyvitamin D (calcitriol),
alters cell behaviour by up- and down-regulating the transcription [
WP] of dozens or hundreds of genes. The Vitamin D Receptor molecule is best thought of as the "calcitriol" receptor.
Returning to the problems caused by the fact that, when measured in
IUs, healthy daily intakes of vitamin D3 involve four of five digits,
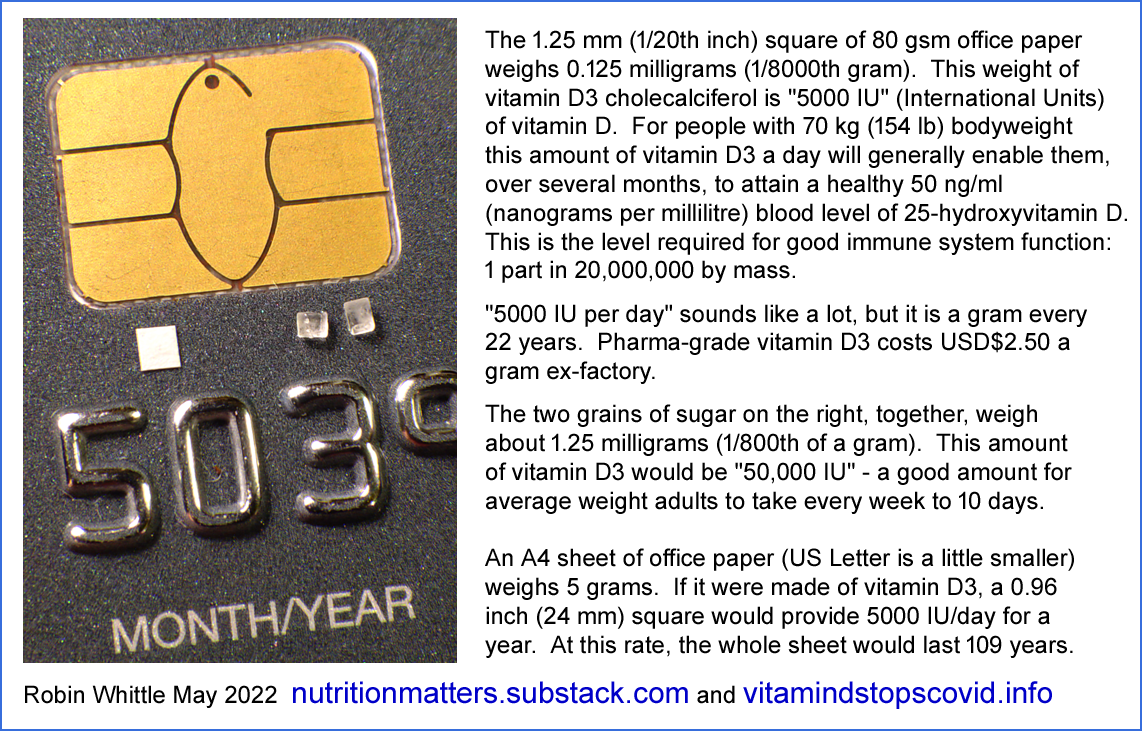
here are some notes on the physicality of
0.125 milligrams 5000 IU of vitamin D3, which is a healthy daily intake for a 70 kg non-obese person:
This is 1/8000 of a gram, about 1/3rd the mass of a poppy seed.
This is the same mass as that of a
1.25 millimetre square of 80 gsm office paper. (A square with 1/20th of an inch sides.)
An A4 [WP]
sheet of office paper weighs 5 grams. (US Letter size is a little
smaller.) If we think of this as being made of vitamin D3 cholecalciferol, a 70 kg
person not suffering from obesity could healthily chomp through this sheet at
one 1.25 mm square per day, consuming the whole sheet after 109
years. Two grains of ordinary table sugar weigh about 1.25 mg,
which as D3 is 50,000 IU.
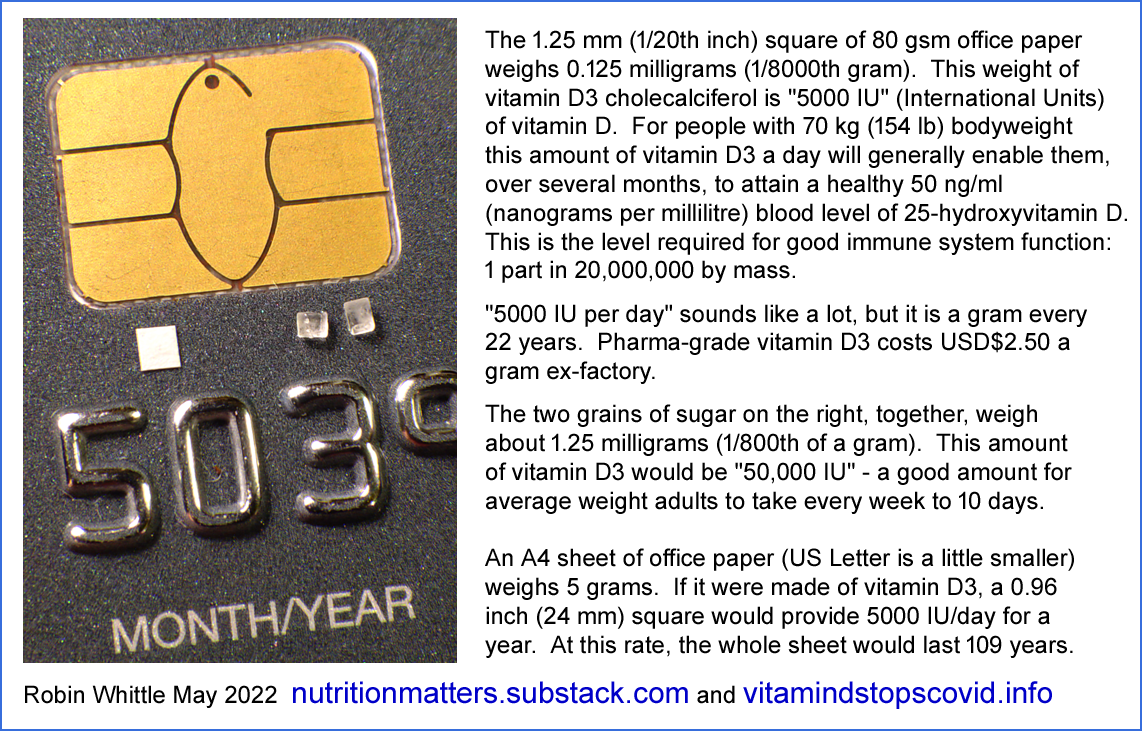
Another quantity worth visualising is the total amount of vitamin D3 a person would consume, over
80 years, when following the UK government's current advice of
0.01 mg 400 IU a day. (For white people this is advised only in winter-spring, but let's assume they took it every day.) The total is
0.293 grams. This is the mass of
18 grains of jasmine rice. The ex-factory cost of this vitamin D3 would have been about
£0.60.
This supports Prof. Martin Hewison's assessment (in the Introduction,
above) of the UK government's guidance: "Keep calm and take
vitamin D (but make sure that it's the lowest dose possible)."
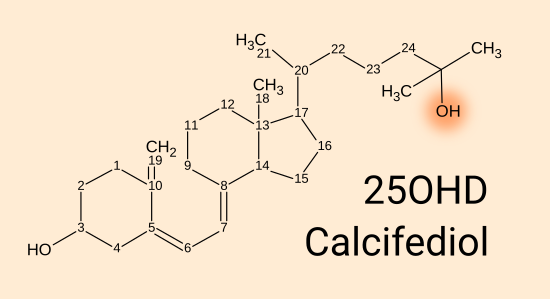
2.2 25-hydroxyvitamin D calcifediol = 25(OH)D
For brevity, I will generally refer to this compound as
25(OH)D.
It is also sometimes referred to as calcidiol, which is a term best
avoided, since it looks and sounds too much like "calcitriol".
Although very small quantities of 25(OH)D may be consumed in food, such
as in the livers of fish, it is not generally regarded as a nutrient or
a vitamin.
Oral (or perhaps intramuscular or intravenous) calcifediol is, however,
a crucial method of boosting circulating 25(OH)D levels, in 4 hours or
so, for clinical emergencies such as COVID-19, sepsis, Kawasaki
disease, MIS-C etc. Although medical treatment is beyond the
scope of this Call for Evidence, the tremendous benefits of this
therapy are discussed in a later section
#4.7, because they establish beyond
doubt how crucial the circulating 25(OH)D level is to the
function of the immune system.
In ordinary human life, 25(OH)D is produced by the hydroxylation of
vitamin D3 - by replacing a hydrogen at the 25th carbon with an
oxygen-hydrogen hydroxyl group. This makes it more water soluble
and gives it a totally different role in the body.
This hydroxylation takes place primarily in the liver, over a period of
days, though to some extent it can also occur in cells elsewhere in the
body. A bolus dose of D3 (such as 10 mg 400,000 IU for 70
kg body-weight) raises 25(OH)D levels in, very approximately, 4 days -
due to the limited amount of the hydroxylation enzyme in the liver and
elsewhere.
25(OH)D has a relatively long half-life in the bloodstream. It
may also be stored to some extent in tissues. At lower levels,
its half-life is several months. Self-limiting mechanisms
(primarily a 24-hydroxylase enzyme, whose activity scales with
increasing 25(OH)D levels) destroy some 25(OH)D and so make it
increasingly difficult to raise its level in the bloodstream, as the
level rises. At higher levels, such as 150 ng/mL (375 nmol/L),
the half-life is a week or two.
25(OH)D is present in the bloodstream in three arrangements. According to:
85% of serum 25(OH)D is strongly bound to Vitamin D Binding Protein (VDBP) [
WP] molecules. This evolved from the albumin [
WP] proteins, which are the most common proteins in the blood plasma..
15% is more loosely bound to albumin proteins.
0.03% is unbound, freely in solution in the plasma.
25(OH)D can diffuse passively across cell membranes. However, its
transport into kidney cells is via an active process which brings it into the cell when it is bound to VDBP.
Vitamin D blood tests measure the total amount of 25(OH)D in the
bloodstream, bound and free. It is also possible to measure just
the free portion, but this is less frequently used in clinical practice.
Here we encounter two alternative systems of units:
- ng/mL = nanograms per
millilitre. This is billionths of a gram of 25(OH)D per gram of
blood plasma [WP]
- the 95% water fluid which makes up 55% of the volume of the blood,
the other 45% comprising blood cells. For instance, 50 ng/mL is
one part 25(OH)D by mass to
20,000,000 parts by mass of plasma.
- nmol/L - nanomoles per
litre. A mole is an SI unit representing a particular number of
molecules: about 6 to the power 23. A nanomole is a billionth of
this, so it is, precisely, 602,214,000,000,000 molecules.
The conversion factor with the mass of the 25(OH)D molecule is about 2.5, so 125 nmol/L 25(OH)D is the same as 50 ng/mL 25(OH)D.
nmol/L is most commonly used in the UK, Canada, Australia and New Zealand.
The level of 25(OH)D in the blood plasma or anywhere else does not
signal anything within the body. While many cell types work best
with a sufficiently high level of circulating 25(OH)D, this level is
not signaling information - it is just providing the chemical precursor
required for proper cellular operation.
25(OH)D never acts as a hormone.
25(OH)D does not bind strongly to the Vitamin D Receptor (VDR).
The level of 25(OH)D is the best measure of a person's total "vitamin D
sufficiency", since vitamin D3 is converted, over a period of days to
a week, to the longer-lasting 25(OH)D which supplies the bodily systems
which we are most interested in:
- The kidneys, in which the 1-hydroxylase enzyme, the activity of
which is tightly controlled by the parathyroid hormone, converts
25(OH)D to a very low level (such as 0.045 ng/mL vitamindstopscovid.info/02-autocrine/#02-nothorm) of circulating 1,25-dihydroxyvitamin D,
which acts as a hormone (endocrine signaling agent) to control the
activities of multiple cell types in distant parts of the body for the
purpose of regulating calcium-phosphate-bone metabolism.
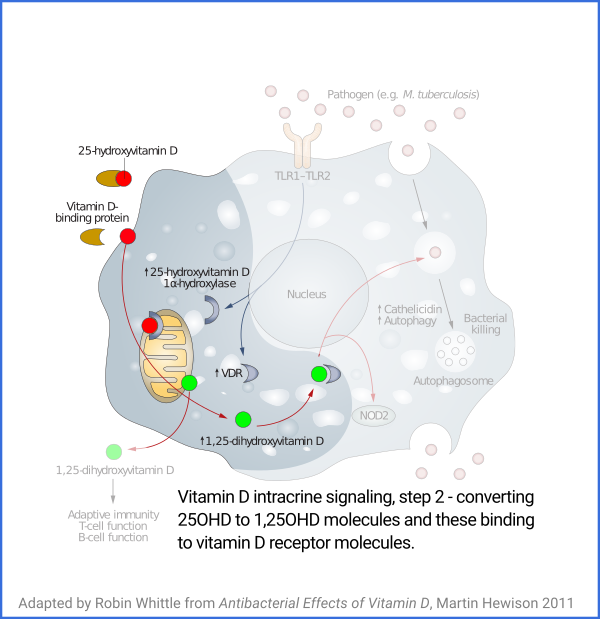
- An unknown number of cell types, including many immune cells,
which are extra-renal (not in the kidneys) and which can hydroxylate
25(OH)D to 1,25-dihydroxyvitamin D. This
1,25-dihydroxyvitamin D does not act as a hormone. Such cell types
may do this for one or both of these purposes:
a - So the 1,25-hydroxyvitamin D binds to VDR molecules inside the same cell. This is properly known as intracrine signaling,
but it is also sometimes referred to as autocrine signaling. (Autocrine
signaling involves a receptor on the outside of a cell binding to, and
so detecting, molecules generated within the cell. There are no
known instances of this, but since "autocrine" was a common term which
roughly described the actual process, it has sometimes been applied to
what Martin Hewison and colleagues described as intracrine signaling.)
b - So some of the 1,25-dihydroxyvitamin D diffuses to nearby cells and affects their behaviour. This is paracrine signaling
and is used by some types of immune cell to affect other types
nearby. Except when immune cells operate pathologically, such as
in granulomatous disorders such as sarcoidosis, this diffusion does not significantly raise
the much lower level of hormonal 1,25-dihydroxyvitamin D in the
bloodstream.
It is important to note that 25-hydroxyvitamin D based intracrine and
paracrine signaling are not continual processes. The
25-hydroxylation of 25(OH)D to 1-25-dihydroxyvitamin D in an individual
cell only occurs after a particular condition has been detected by that
cell. Each cell type which is capable of doing this
conversion does so in response to its own, cell-type-specific,
condition. The purpose of these signaling systems is for that
cell, after having detected that condition, to change the behavior of
itself and some types of cell (usually of a different type to the one
producing the 1,25-dihydroxyvitamin D) which are nearby.
2022-07-09 update:
In
granulomatous disorders such as sarcoidosis, some immune cells continually convert
25(OH)D into excessive quantities of 1,25-dihydroxyvitamin D, some of which
leaks from the cells and goes into
circulation, adding to the hormonal 1,25dihydroxyvitamin D. If this
happens to a small degree, the kidneys remain in control of this hormonal level
by producing less of it. Larger contributions from this pathological
immune cell production of 1,25-dihydroxyvitamin D may cause hormonal levels to
rise significantly above what is required for proper calcium-phosphate-bone
metabolism. This can raise the level of circulating calcium ions, which
should be very tightly controlled. The result, in extreme cases, may be
calcification of the arteries and other tissues.
This has lead to a long-standing "conventional wisdom" that in these
disorders it is necessary to lower 25(OH)D levels in order to reduce the
ability or the aberrant immune cells to produce so much 1,25-dihydroxyvitamin
D.
However, Kamphuis et a. 2014 report that patients with sarcoidosis do better
with higher 25(OH)D levels.
Calcium
and Vitamin D in Sarcoidosis: Is Supplementation Safe?
Lieke S Kamphuis, Femke Bonte-Mineur, Jan A
van Laar, P Martin van Hagen, Paul L van Daele
Journal of Bone and Mineral Research 2014-04-18
doi.org/10.1002/jbmr.2262
(Paywalled.)
sci-hub.se/10.1002/jbmr.2262
This supports the hypothesis that the cells are misbehaving due to
immune dysregulation which is due, in part, to some immune cells -
probably not the ones producing the excessive 1,25-dihydroxyvitamin D -
not getting sufficient 25(OH)D to run their intracrine and perhaps
paracrine signaling systems, which would make them incapable of
properly changing their own behaviour in response to a particular
condition they detect, and also incapable of regulating the activities
of other cells. The excessive
consumption of 25(OH)D by the aberrant cells may result in localised
and/or body-wide depletion of 25(OH)D which may further drive the
dysregulation which causes the aberrant conversion.
A major failing of the vitamin D research literature is that there is
no peer-reviewed journal article which explains vitamin D based
intracrine (AKA autocrine) and paracrine signaling. So I made my
own tutorial for this purpose:
vitamindstopscovid.info/02-intracrine/ . Here is one of the illustrations, but please refer to this page for the full explanation.
While the kidneys, working with the parathyroid gland [
WP] and osteocytes [
WP] in the bone itself, continually maintain a tightly controlled,
circulating, level of 1,25-dihydroxyvitamin D, for the crucial hormonal
regulation of calcium-phosphate-bone metabolism, the cell types, and
individual cells, which use 25(OH)D for intracrine and/or paracrine signaling use it in a completely different way.
All medical professionals understand the kidney system, which is a
straightforward hormonal, endocrine signaling, system. To the
extent that they are aware of the importance of "vitamin D" to the
immune system, it is a common and serious mistake for them to assume
that the immune system also works on a hormonal, endocrine,
basis. It is not surprising that they think this, since one
has to look very carefully at a handful of journal articles to discern
that this is not the case.
This leads to a common mistaken belief that the immune system works
better with higher levels of circulating 1,25-dihydroxyvitamin D.
It doesn't.
Leaf et al. 2014
tried forcibly raising circulating 1,25-dihydroxyvitamin D to treat
sepsis, and found no benefit. Such treatments are likely to
disturb blood plasma calcium levels, which must be maintained within very
narrow limits.
Vitamin D's importance to the immune system cannot be understood
without clearly recognising that the use of 25(OH)D by multiple types
of immune cells works on entirely different principles to those which
the kidney uses:
- In 25-hydroxyvitamin D based intracrine and paracrine signaling, the hydroxylation conversion process is not continual. It
is only activated in a particular cell when that individual cell
detects a particular condition has occurred. What the condition is
varies from one cell type to the next.
- In the case of intracrine (autocrine) signaling, the effect of
the just-produced 1,25-dihydroxyvitamin D is to bind to VDR molecules
in the same cell, with the bound complexes altering gene expression,
and so protein synthesis and the behaviour of the entire cell, in ways
which vary from one cell type to the next.
- Likewise,
for those cell types which respond to diffused
1,25-dihydroxyvitamin D (produced as just described, in a cell of one
type, and which diffuses from that cell into the fluid surrounding
it) which reaches them as a paracrine agent (the
level of this is much higher than the hormonal 1,25-dihydroxyvitamin D
background), the way this changes the behaviour of the cell varies
greatly from one cell type to the next.
The way the immune system uses 25(OH)D is completely separate from, and
functions on entirely different principles, for entirely different
purposes, to the way the kidneys use it.
All medical professionals -
and
immunologists, endocrinologists, virologists, vaccinologists,
epidemiologists and public health officials - need to understand, in
broad terms, how full immune system competency depends:
- Entirely on there being good, 50 ng/mL (125 nmol/L) or greater levels of
circulating 25(OH)D. This does not signal information to any cell. It
simply supplies sufficient 25(OH)D to all the cells which need it, and
maintains this supply when it is consumed within each cell when its
intracrine/paracrine signaling system is activated.
- Not at all on the very low and stable level of circulating, hormonal, 1,25-dihydroxyvitamin D.
Once this is understood, and it is recognised that toxicity may only
become a concern for 25(OH)D levels of 150 ng/mL (375 nmol/L ) or above,
it can be seen that proper immune system health can only be assured
with 25(OH)D levels of 50 ng/mL (125 nmol/L) or more, and that this or
double to probably triple this level, will not cause toxicity, or
disturb the hormonal regulation of calcium-phosphate-bone metabolism.
Please refer to this recent review of vitamin D based intracrine and
paracrine signaling by Professor Martin Hewison and colleagues.
Fletcher et al. address autoimmune diseases, but the same mechanisms enable
immune cells to respond correctly to produce healthy innate and
adaptive immune responses to viral, bacterial and fungal pathogens.
Most of the early work on vitamin D based intracrine and paracrine
signaling was done by Prof. Hewison and colleagues in the mid to late
2000s, with macrophages [
WP] and dendritic cells [
WP].
#chauss
A spectacular advance in this field, cited in the above article, is the work of
Chauss et al. who researched the failure of Th1 regulatory
lymphocytes [
WP] from the lungs of hospitalised COVID-19 patients to turn
off their pro-inflammatory startup program, when they detected the
external signal to do so. They should turn this off and
transition to an anti-inflammatory shutdown program.
This
failure was found to be due largely or solely to inadequate supplies of
25(OH)D:
Autocrine vitamin D signaling switches off pro-inflammatory programs of Th1 cells
Daniel
Chauss, 26 other authors and (lead authors) Majid Kazemian and Behdad Afzali
Nature Immunology
2021-11-11
www.nature.com/articles/s41590-021-01080-3
This is a dense cell biology article, which likely exceeds the
expertise and/or patience of most medical doctors. You may wish to
refer to my summary of the preprint version of this article,
aminotheory.com/cv19/icu/#2021-Chauss . The term "autocrine" is not quite correct - the processes described in this article are properly known as
intracrine signaling.
"Autocrine" means the ligand produced in the cell is detected by a
receptor on the outside of the cell, but with 25(OH)D >>>
calcitriol signaling, the receptor molecules are inside the cell.
The proper functioning of the immune system depends on 50
ng/mL (125 nmol/L) or more 25(OH)D circulating in the blood serum. Since most
people do not naturally get enough vitamin D to attain this,
the health
of all humanity depends on most doctors, immunologists understanding this by familiarising
themselves with vitamin D based intracrine (AKA autocrine) and
paracrine signaling, so they can advise governments and individuals on
the best way of attaining these levels.
The above two articles are crucial to developing this understanding.
Neither refers directly to the requisite 25(OH)D level, but you can see
from Quraishi et al.'s graph (above
#00-quraishi and
discussed below further) and from numerous observations, such as of
25(OH)D level vs. COVID-19 severity, that 50 ng/mL (125 nmol/L) is the
proper minimum level, NOT 30 ng/mL (75 nmol/L) recommended by the Endocrine Society and especially NOT the
lousy 20 ng/mL (50 nmol/L) level of vitamin D deficiency which is
currently recommended by the UK and most or all other governments.
The Endocrine Society's recommendation for 30 ng/mL (75 nmol/L)
25-hydroxyvitamin D as the threshold of vitamin D deficiency was
published in 2011 and remains current to this day:
Evaluation, Treatment, and Prevention of Vitamin D Deficiency: an Endocrine Society Clinical Practice Guideline
Michael F.
Holick, Neil C.
Binkley, Heike A. Bischoff-Ferrari, Catherine M. Gordon, David A.
Hanley, Robert P. Heaney, M. Hassan Murad and Connie M. Weaver
Journal of Clinical Endocrinology & Metabolism
2011-07-01
academic.oup.com/jcem/article/96/7/1911/2833671
On the dangers of
toxicity, due
to destablising blood plasma calcium levels (which must be tightly regulated)
due to excessive 25-hydroxyvitamin D, the Endocrine Society guidelines
state:
Although it is not known what the safe upper value for 25(OH)D is for avoiding hypercalcemia, most studies in children and adults have suggested that the blood levels need to be above 150 ng/mL [375 nmol/L] before there is any concern.
Unfortunately, the next sentence, without any justification, provides a
33% lower threshold which many doctors have regarded as an upper safety
limit:
Therefore, an UL of 100 ng/mL [250 nmol/L] provides a safety margin in reducing risk of hypercalcemia.
This arbitrarily low threshold is one of the reasons for unjustified concerns about vitamin D toxicity.
Calcifediol (the pharmaceutical name for 25-hydroxyvitamin D) is produced industrially, in China and Europe, primarily
for agricultural animals. Smaller quantities of pharma-grade
calcifediol are produced, using a yeast-based process with UV-B, by DSM
in Europe
www.dsm.com . DSM sell it without prescription as a nutrient - a
nearly instantly absorbed alternative to vitamin D3 for raising and
sustaining 25(OH)D levels. Spanish company Faes Farma sell a
prescription form in Spain and Italy.
Calcifediol was used to rapidly boost 25-hydroxyvitamin D levels in
hospitalised COVID-19 patients, with great success. See Castillo
et al. 2020, below:
#castillo.
While calcifediol is a uniquely rapid way of boosting 25(OH)D levels in
clinical emergencies, I know of no evidence which indicates it is more
suitable for long-term nutrition than vitamin D3 cholecalciferol.
It is not normally regarded as a nutrient. It is not a
drug. Nor is it a vitamin. It is not a hormone since its
level in the blood does not convey information - it does not signal
anything to any cells.
The concept of International Units is not normally applied to
calcifediol. However, in the long term, in regular daily use, 100
micrograms (for instance) of calcifediol per day is about as effective
at raising 25(OH)D as (very approximately) 400 micrograms per day of
vitamin D3. Even with this greater efficiency per unit
mass, calcifediol's more than 4 times higher price makes it less cost
effective than vitamin D3.
2.3 1,25-hydroxyvitamin D calcitriol = 1,25(OH)2D
For brevity, I will generally refer to this as
1,25(OH)2D or calcitriol.
(In conversation I refer to the three compounds as:
- vitamin D3
- 25-hydroxyvitamin D (or as "calcifediol" if it is a pharmaceutical be ingested or injected)
- calcitriol
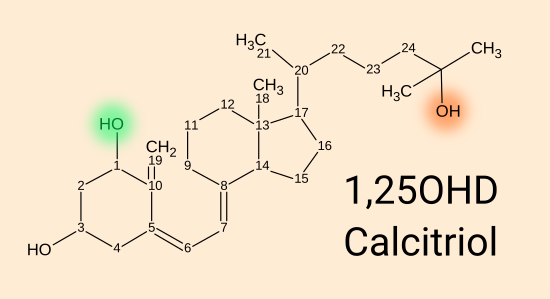
Most of what you need to know about calcitriol is in the previous sub-section.
It is produced in multiple cell types by the 1-hydroxylase enzyme
attaching a hydroxyl group in place of the hydrogen at the number 1
carbon of 25(OH)D.
This completely alters the molecule's behaviour. 1,25(OH)
2D
calcitriol binds strongly to the VDR (vitamin D receptor) molecule. So
it often referred to as "activated vitamin D". However, this
terminology is based on the mistaken notion that all three compounds
are somehow really "vitamin D".
The kidneys maintain a very low, stable level of calcitriol
circulating in the bloodstream, where it functions as a hormone,
enabling the kidneys (responding to the parathyroid hormone level and FGF-23 [
WP] emitted by osteocytes) to
control the activity of multiple cell types all over the body regarding
the absorption and excretion of calcium and phosphate, the levels of
these in the bloodstream and the constant building and destruction of bone, by
osteoblasts and osteoclasts respectively, which is essential for bone
health. All medical professionals, immunologists etc. understand
this well.
Calcitriol can also function, as described above, as an intracrine
(AKA, incorrectly as "autocrine") agent and as a paracrine agent.
In the bloodstream, hormonal calcitriol (whose level is controlled by
its production in the kidneys, even if some of the circulating
calcitriol
leaked from cells which produced it as an intracrine/paracrine agent)
has a half life of a day or less. This hormonal level is
typically around 0.11 nmol/L 0.045 ng/mL. (See
vitamindstopscovid.info/02-intracrine/#02-nothorm for references,)
The kidneys can generally maintain this as long as they have something
in the order of 50 nmol/L 20 ng/mL circulating 25(OH)D, though they may do it better with higher levels. So the current UK
standard of vitamin D sufficiency (50 nmol/L 25(OH)D is reasonable for
bone health. However, this standard is only 40% of what is
required to assure proper immune system function.
The enzymes in the bloodstream which degrade calcitriol are also active
in cells in which it is used as an intracrine / paracrine agent.
This mops up calcitriol
quickly, ensuring that once its intracellular production ceases, its
activation (binding to) of VDR molecules also ceases in a timely manner, turning off
the changes to cell behaviour which occurred due to many VDR molecules
being activated. (The precise details of how the bound calcitriol-VDR
complexes work within the nucleus to alter gene expression are
complex, beyond the scope of this submission and need not be
understood
by medical professionals. I am not sure of the lifetime of the
bound complexes. However, the nature of the timely
responses which result from intracrine and paracrine signaling
means the complexes must have a limited lifetime.)
Calcitriol is not a nutrient, a vitamin or a drug. It
can be used as a medication to make up for the failure of kidneys to
maintain the proper hormonal calcitriol level.
While it is possible to clinically measure the level of calcitriol in the
bloodstream, this gives us information about the regulation of
calcium-phosphate-bone metabolism, and tells us nothing about the
operation of the immune system.
All the above material about calcium-phosphate-bone metabolism is well known to medical professionals and is not contentious.
The material about the immune system is based on research in the last
15 years, which only partly covers the full scope of the vitamin D
compounds in the immune system and in the still less researched cell
types outside the immune system which also use vitamin D based
intracrine and/or paracrine signaling. This material is generally
not known by medical professionals, and there are many MDs and
researchers who publish research articles on vitamin D who have little
or no awareness of these observations and principles.
However,
humanity absolutely depends
on good 25(OH)D levels - and will only have these levels in general
once most health professionals, immunologists, virologists etc. develop
a proper understanding of vitamin D based intracrine/paracrine
signaling, at least as it is used in the immune system.
#03-uk-low
3 Terribly low 25-hydroxyvitamin D levels in the UK
Most UK citizens, all year round, have
25-hydroxyvitamin D levels far below the 50 ng/mL (125 nmol/L) needed for
proper immune system function. This has pervasive negative health
consequences from early in-utero development to old age - as discussed
in Section 4.
Section 5 outlines how current, completely inadequate, UK government vitamin D guidance arose.
The only solution to this is for most people to properly supplement
vitamin D3, all year round, with (in the absence of medical advice to
the contrary) the daily intake quantity being set by a ratio
of body-weight and whether the person suffers from obesity. This is
the subject of section 6 below.
Section 7 explains why healthy 25-hydroxyvitamin D levels cannot be
attained through food fortification alone - and furthermore why all
government efforts should be directed to supplementation, and none to
fortification.
Section 8 discusses how government standards and support for education
and provision of proper supplemental vitamin D can solve these problems
and ensure that most UK citizens have the 25-hydroxyvitamin D levels
they need for full immune system health.
The following graph depicts UK BIOBANK observations of 40 to 69 year olds between 2006 and 2010:
Sutherland et al.
2020:
sci-hub.se/10.1016/j.clnu.2020.11.019 .
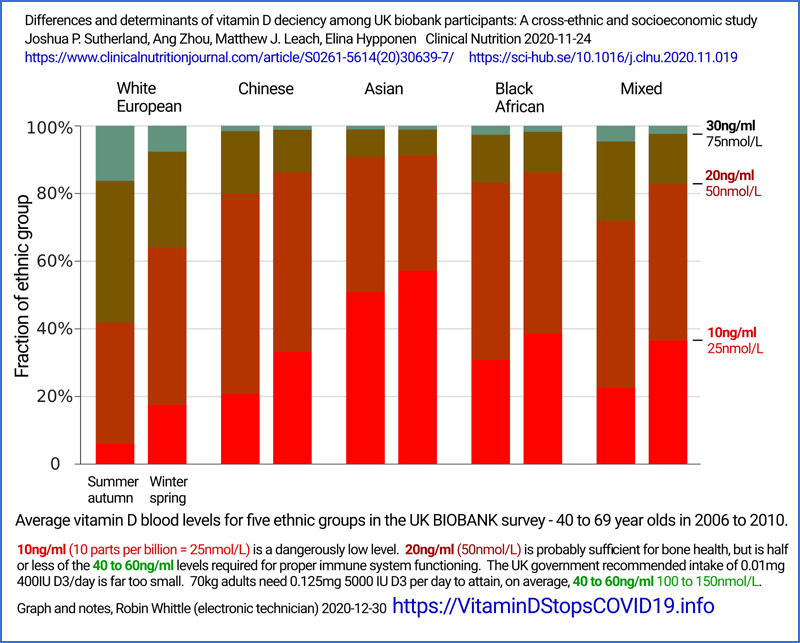
Hopefully present-day levels in this and other age-groups would be
higher, but we need not just marginal change from the levels depicted
above, but a nation-wide transformation.
Even among white-skinned people, only about 10% of the subjects had
25(OH)D levels above 30 ng/mL (75 nmol/L) in winter-spring. So it is
reasonable to assume that only 2 or so percent of these people had
25(OH)D levels of 50 ng/mL (125 nmol/L) or more, which their immune systems need
to function properly. The situation was far worse, all year
round, for all those people surveyed who had darker skin and/or whose
culture and clothing resulted in less direct, high-elevation, sunlight
reaching their skin than the already low amount which, on average,
reaches Caucasians' skin.
From the same article:
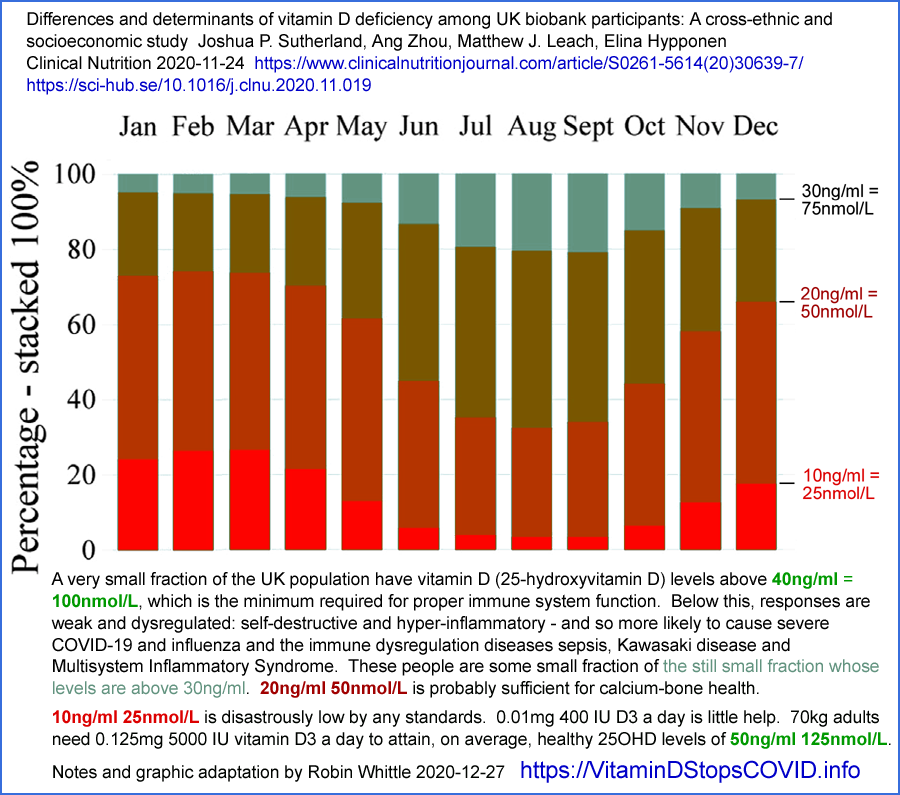
Here is another analysis of the BIOBANK data, from:
Very high prevalence of 25-hydroxyvitamin D deficiency in 6433 UK South Asian adults: analysis of the UK Biobank Cohort
Andrea L.
Darling, David J. Blackbourn, Kourosh R. Ahmadi and Susan A. Lanham-New.
British Journal of Nutrition
2020-07-22
doi.org/10.1017/S0007114520002779
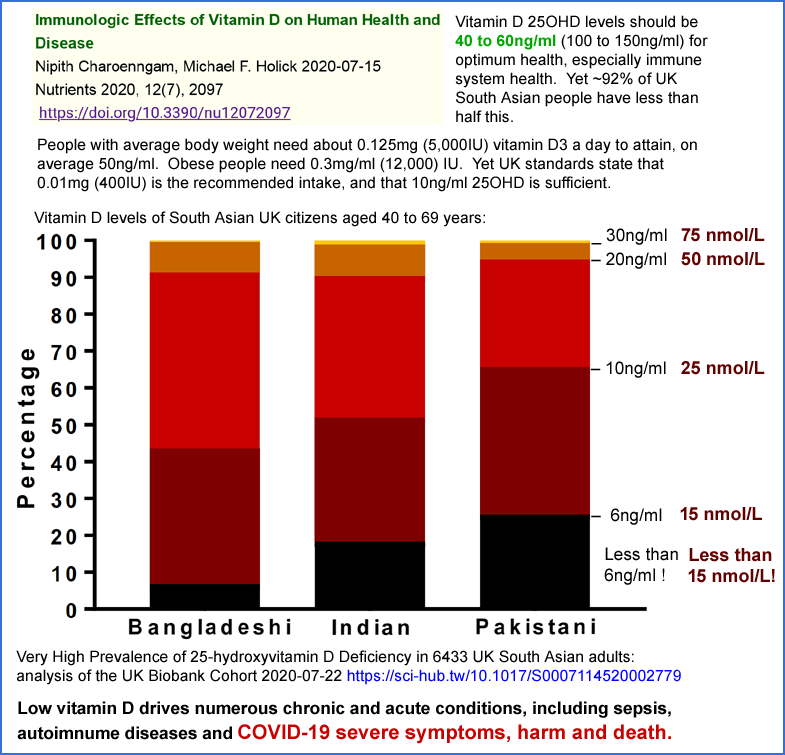
About half of these people have 1/5th or less of the 25(OH)D their immune systems need to work properly.
The impact of the UK's great distance from the equator - 50° to 59° -
is evident even within the British Isles in these maps depicting
average 25(OH)D levels:
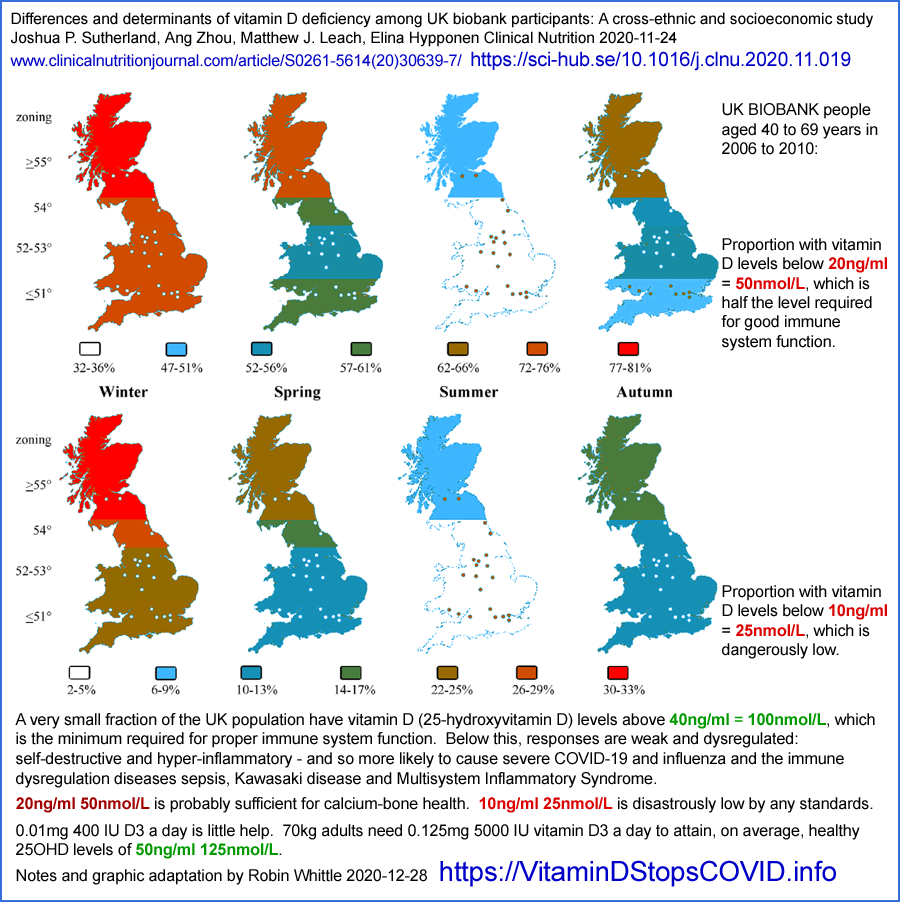
Here is another depiction of the seasonality of average
25-hydroxyvitamin D levels in the UK, again from BIOBANK data.
Here I have copied the vector-based graphs from the article and
enlarged and annotated them, so they are larger but still precise. This is from
Raisi-Estrabragh et al.
2020 doi.org/10.1093/pubmed/fdaa095 .
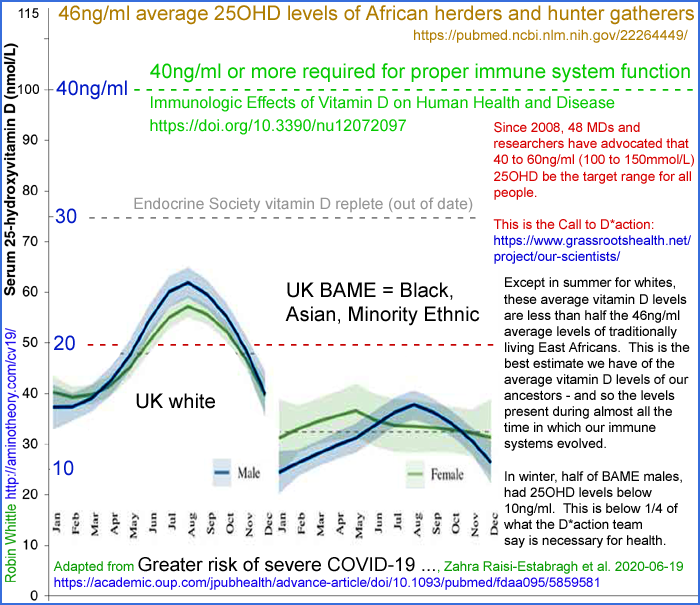
Note that this chart doesn't extend quite to the 50 ng/mL (125 nmol/L)
level now widely recognised as required for proper immune system
function. I made this chart in mid-2020, before becoming aware
of Quraishi et al. 2014. According to this BIOBANK data,
average white 25(OH)D levels briefly approach
half that level. Average BAME levels are a
quarter of what is required for good immune system health.
#israel
The impact of sun-avoidant clothing and cultural norms is especially
evident in the following histograms depicting distribution of 25(OH)D
levels in Israel, from:
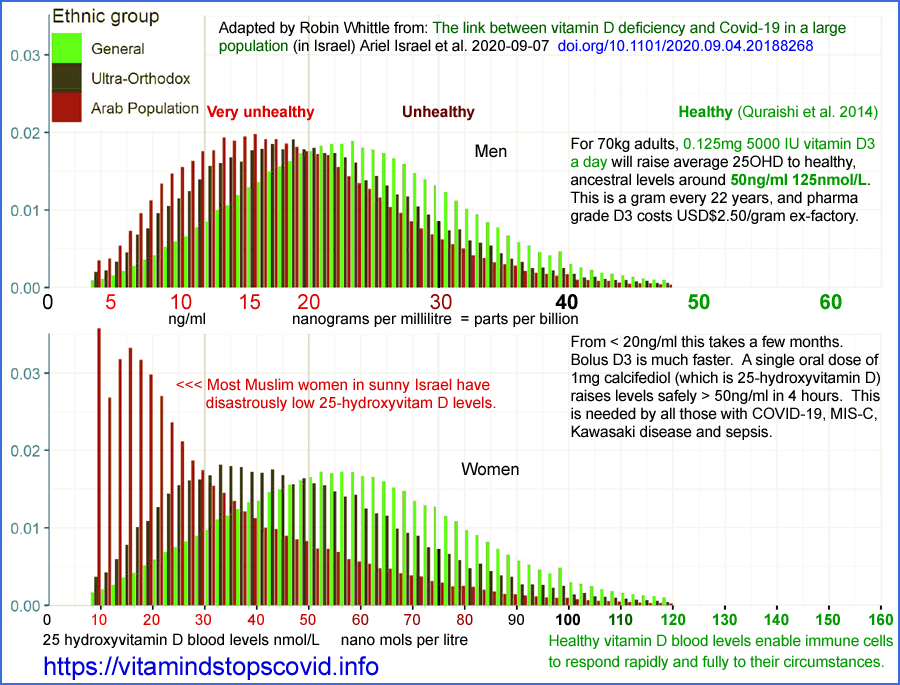
(I reproduce these histograms as part of the Dror et al. infographic at the top of this page.)
Despite being much closer to the equator than UK residents - 30° to 33° - almost no
Israelis, who mainly have white skin, attain 50 ng/mL (125 nmol/L)
25(OH)D. People are wisely advised to avoid direct UV-B exposure in order to protect against skin cancer.
My reason for including these histograms is to draw attention to the
extreme ill-effects of cultural practices and clothing which even
further reduce the skin's exposure to UV-B light from the
Sun. Ultra-orthodox men and women of the primarily white
"general" (Jewish) population have somewhat lower 25(OH)D levels,
presumably due to sun avoidant behaviour and clothing.
The same can be said of Arab men, who may also on average have
more melanin-rich skin, and so who create less vitamin D3 cholecalciferol
for any given amount of UV-B skin exposure.
The most striking histogram is that of Arab women. The extreme
preponderance of low 25(OH)D levels with respect to those of Arab men
is surely explained by the proclivity of Arab women in Israel to wear
full body
covering clothing and to avoid sun exposure in general.
The left bar (4 ng/mL 10 nmol/L) for Arab women is higher than the trend
curve because some women have levels below this detection limit.
To whatever extent women in the UK avoid direct high elevation sun
exposure of their skin, for cultural or other reasons, we can expect
their 25(OH)D levels to be even lower than in Israel due to sunlight in
the UK always arriving at lower angles from the horizon, which strongly
attenuates its UV-B content, as well as having more cloudy days and
less warm days in which people are likely to be outside with direct
sunlight falling on their skin .
3.1 Comparing UK 25(OH)D levels with those of our African ancestors
The only indication we have of the 25(OH)D levels of our African
ancestors, prior to the development of modern clothing and migration
far from the equator, is a small series of measurements taken from
traditionally living East
African Maasai herders and Hadzabe hunter gatherers:
Traditionally living populations in East Africa have a mean serum 25-hydroxyvitamin D concentration of 115 nmol/L (46 ng/mL)
Martine F
Luxwolda, Remko S Kuipers, Ido P Kema, D A Janneke Dijck-Brouwer and Frits A J Muskiet
British Journal of Nutrition
2012-01-23
doi.org/10.1017/S0007114511007161
We measured the sum of serum 25-hydroxyvitamin D2 and D3 (25(OH)D) concentrations of thirty-five pastoral Maasai (34 (sd 10) years, 43 % male) and twenty-five Hadzabe hunter–gatherers (35 (sd
12) years, 84 % male) living in Tanzania. They have skin type VI, have a
moderate degree of clothing, spend the major part of the day outdoors,
but avoid direct exposure to sunlight when possible.
The average 25(OH)D level was
115 nmol/L 46 ng/mL.
(In May 2023 I analysed the data
in this article and produced a histogram, which appears in the above
Dror et al infographic at the top of this page, a more detailed version
of which is: 1-Dror-Israel-14-framed.png. Please write to me if
you want the details of how I calculated the coordinates of this
histogram.)
Fitzpatrick skin type VI (6, of 1 to 6) is the darkest type. Images from the UK:
www.sungoddesskin.co.uk/what-skin-type-are-you/ Sachdeva 2009:
Dark brown to black. Never burns, tans profusely.
From this we can see that white-skinned people living in sunny Israel
are highly 25-hydroxyvitamin D deficient with respect to the African
people sampled by Luxwolda et al. - and that (without proper vitamin D3
supplementation) almost everyone in the UK is even more deficient.
This sample of 60 Africans is the best information we have about
ancestral 25(OH)D levels. We should not assume that these
African levels are optimal for all people, such as those in the UK
today. Vitamin D3 is a vital compound for general health, but -
since there is very little in food - without supplements it can only be
obtained by exposing the inner layers of the skin to UV-B radiation
around 290 to 315 nanometres wavelength (in order to get the necessary light around 295 to 297 nm), which always damages DNA and
so raises the risk of skin cancer.
This cancerous trade-off in producing vitamin D3 is an argument
that the
long-evolved production quantities (limited in our African ancestors by
intense melanin, evolved for this purpose), and so the resulting levels
of
circulating 25(OH)D, are lower than the levels which would most benefit
health. Humanity may arguably have evolved higher 25(OH)D levels
if the requisite vitamin D3 could have been obtained without risk of
skin damage and cancer.
3.2 Good 25-hydroxyvitamin D levels essential for pregnancy and childbirth
2024-11-25: See also the additional
research on preeclampsia, pre-term birth and the incidence of
preeclalmpsia raising the risk of the mother suffering early-onset
dementia (before 65 years), discussed at:
Here is a graph and some quotes from an important UK study:
Failure of national antenatal vitamin D
supplementation programme puts dark skinned infants at
highest risk: A newborn bloodspot screening study
Suma Uday, Sunia Naseem, Jamie Large, Russell Denmeade,
Philippa Goddard, Mary Anne Preece, Rachel Dunn, William
Fraser, Jonathan C.Y. Tange, Wolfgang Högler
Clinical Nutrition 2020-12-11 (In press.)
www.sciencedirect.com/science/article/abs/pii/S0261561420306671
(Paywalled.)
sci-hub.se/10.1016/j.clnu.2020.12.008
Vitamin D deficiency is highly prevalent in all babies born in the UK, especially in winter months.
The high proportion of dark-skinned infants with low vitamin D status,
demonstrates the failure of the UK's national antenatal supplementation
programme in protecting these ethnic groups, who are well recognised to
be at a high risk of vitamin D deficiency.
This is from researchers, who like many doctors in the UK, consider 20 ng/mL (50
nmol/L) 25(OH)D to be "sufficient". The situation is more
alarming still when it is recognised that 50 ng/mL (125 nmol/L) is the
proper standard of sufficiency.
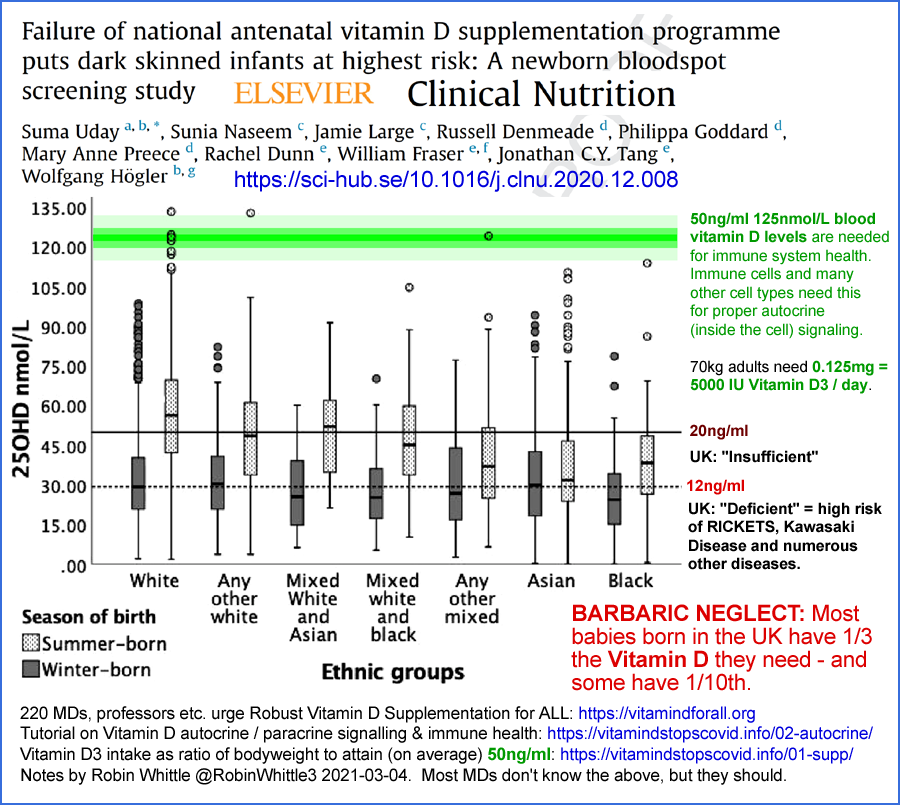
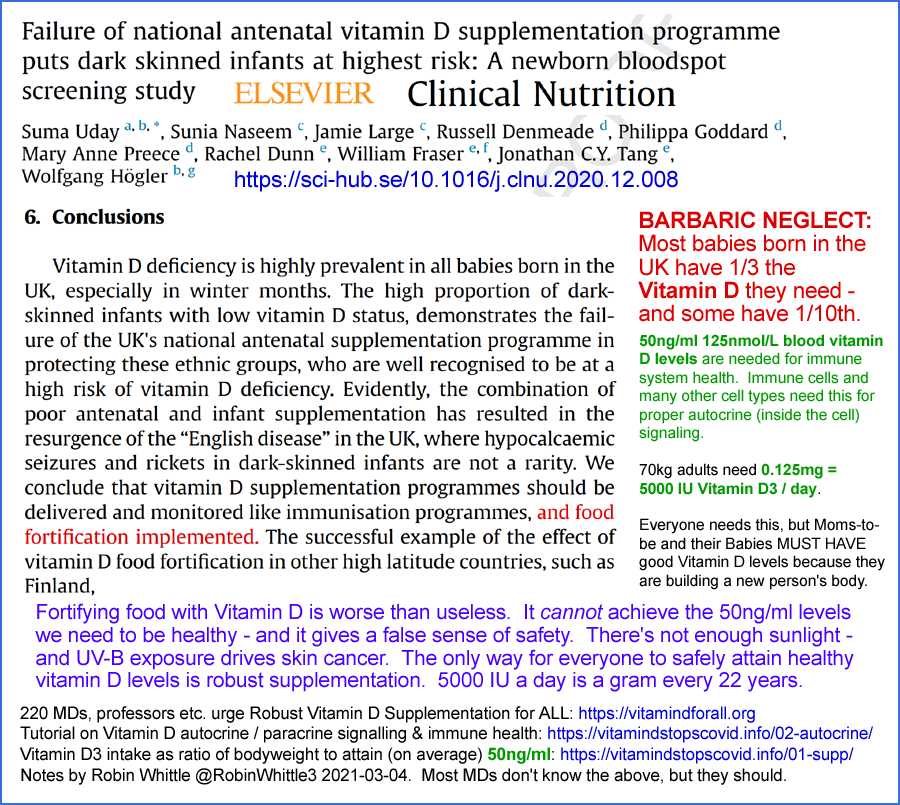
(New material added 2022-12-05.)
The next graph is from an RCT involving
either 0.01 or 0.11 mg (400 or 4400 IU) vitamin D3 a day with pregnant
women (though some may have been taking their own vitamin D3
supplements), initiated in gestational weeks 10 to 18. Women who
suffered from hypertension were excluded. Rates of preeclampsia [
WP]
were no lower in the 4400 IU/day treatment group than in the 400 IU/day
group. However, there was a strong anti-correlation between
25-hydroxyvitamin D levels and rates of pre-eclampsia.
Preeclampsia affects 2 to 8% of pregnancies worldwide.
It involves an onset of high blood pressure (hypertension) and protein
in the urine, after the 20th week of pregnancy. If left
untreated, seizures (eclampsia) occurs along with many other adverse
outcomes.
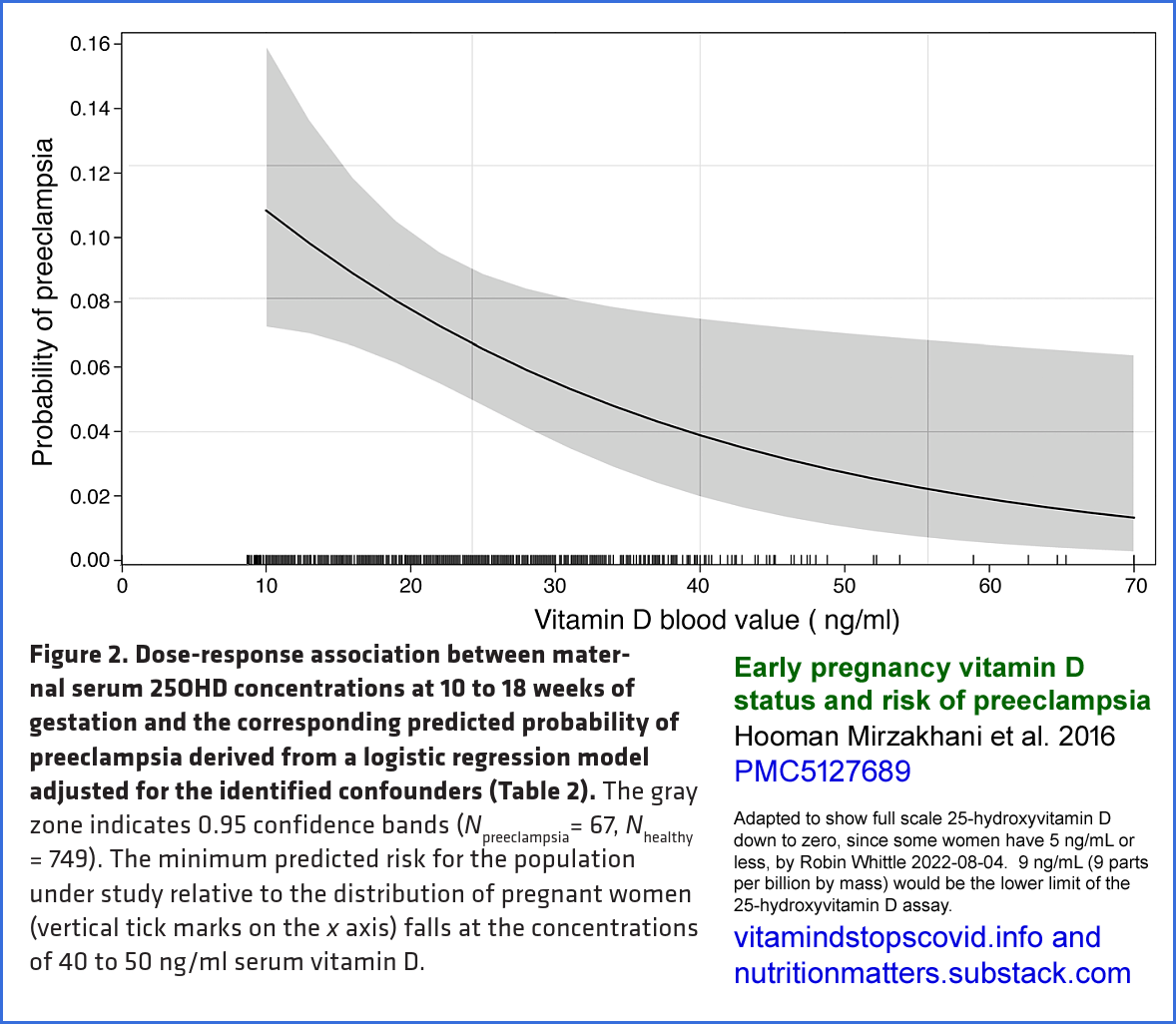
Early pregnancy vitamin D status and risk of preeclampsia
Hooman
Mirzakhani and 22 others, including Bruce W
Hollis.
Journal of Clinical Investigation
2016-09-16
www.jci.org/articles/view/89031
A Google Scholar
search
shows a strong relationship between preeclampsia and inflammation.
Risk factors include obesity, prior hypertension, older age, and
diabetes mellitus. The
word "eclampsia" is from the Greek term for lightning. The first known
description of the condition was by Hippocrates in the 5th century BC.
In the 400 IU/day vitamin D3 group (basic 400 IU/day plus placebo), at
baseline (weeks 10 to 18) the mean 25-hydroxyvitamin D level was 22.6
ng/mL. This rose 4.2 ng/mL, by the 3rd trimester, to 26.8
ng/mL. In the 4400 IU/day group, the mean level at baseline was
23.3 ng/mL, and rose 15.9 ng/mL to 39.2 ng/mL. It takes months
for 25-hydroxyvitamin D levels to substantially stabilise with daily
intakes like this. It would have been better to give the women a
bolus vitamin D3 dose such as 10 mg 400,000 IU which would raise most
of their levels safely over 50 ng.mL within (very approximately) 4
days. Better still, for (for 70 kg bodyweight) a single oral
dose of 1 mg calcifediol, which _is_ 25-hydroxyvitamin D, would boost
the levels similarly in about 4 hours. Please see
nutritionmatters.substack.com/p/calcifediol-to-boost-25-hydroxyvitamin and
#sjw-article.
However, Mirzakhani et al.'s results indicate that boosting
25-hydroxyvitamin D, slowly - such as with 0.11 mg 4400 IU / day
starting in weeks 10 to 18 - makes no difference to preeclampsia
rates. So rapid boosting would not necessarily make a significant
difference either.
An explanation of this can be found in the hypothesis that while preeclampsia usually occurs after 32 weeks (here quoting
en.wikipedia.org/wiki/Pre-eclampsia) its cause lies in problems with the implantation of the placenta, which occurs much earlier. From
Rana et al. 2019:
Preeclampsia progresses in 2
stages: (1) abnormal placentation early in the first trimester
followed by (2) a maternal syndrome in the later second and third
trimesters characterized by an excess of antiangiogenic factors.
The first trimester is weeks 1 to 12, the second, weeks 13 to 26 and
the third, weeks 27 to birth - which is on average around 40
weeks. From the
Merck Manual, an illustration showing the fetal blood vessels closely intermingled with the maternal blood vessels in the placenta:
"Antiangiogenic factors" are compounds which inhibit the formation of blood vessels.
While the mechanism of abnormal placentation is controversial, animal models have demonstrated that uteroplacental ischemia [lack of blood flow in the mother's blood vessels in the placenta]
drives the hypertensive, multi-organ failure response observed in the
maternal preeclamptic syndrome (stage 2). A number of theories
have been proposed for the placental dysfunction observed in stage 1,
including oxidative stress, abnormal natural killer cells (NKs) at the
maternal-fetal interface, and genetic and environmental factors, though
none have conclusive evidence in humans. However, substantive evidence
supports the idea that the diseased placenta leads to release of soluble toxic factors in the maternal circulation that result in inflammation, endothelial [cells which form the interior lining of blood vessels] dysfunction, and maternal systemic disease.
On this basis, the primary or sole cause of the symptoms of
preeclampsia which begin after week 20 is abnormal development of
intermingled fetal and maternal blood vessels, which were complete in structure -
though not yet fully grown, 12 weeks earlier.
It would not
be surprising if low 25-hydroxyvitamin D levels around week 8,
together with other conditions including general nutrition and genetic
disposition, lead to a faulty pattern of placental blood vessel development.
While it is reasonable to tentatively assume that this faulty
development is largely driven by weakened innate and adaptive maternal
immune responses and/or dysregulated and excessively strong maternal
inflammatory responses (due to low 25-hydroxyvitamin D and/or lack of
helminths
vitamindstopscovid.info/06-adv/#02-helminths),
it would not be surprising if the problems are caused, at least in
part, by some cell-types which are not part of the immune system failing
to build the vascular structures properly, due to lack of
25-hydroxyvitamin D to supply their vitamin D based intracrine and/or
paracrine signaling systems.
Vitamin D based intracrine (and in some cases paracrine) signaling has
only been clearly described in macrophages, dendritic cells (both by
Martin Hewison and colleagues, in the late 2000s) and Th1 lymphocytes
(by Chauss et al. 2021 (
#chauss). However,
it is reasonable to assume that one or both signaling systems are
present in many other cell types - both in the immune system and cell
types unrelated to the immune system.
Ideally I would present a better account of the following, and I plan
to in the future when I find the appropriate references. The
argument is that some large number of cell types are known to have
their gene transcription significantly affected by activated vitamin D
receptor molecules - and that most of these cell types which are not
involved in calcium-phosphate-bone metabolism, are not responding to
hormonal 1,25-dihydroxyvitamin D. So they must be responding to
1,25-dihydroxyvitamin D which is acting as an intracrine and/or
paracrine agent. It is easy to imagine such signaling systems
being used by some cell types to change their behavior when they
partake in, for instance, the development of complex neural structures,
or complex patterns by which two sets of blood vessels, from two
genetically distinct individuals, grow close to each other in what must be a
carefully controlled manner to form the placenta.
Given the reasonably assumed reliance of many cell types on vitamin D
based intracrine and paracrine signaling, both of which enable cells to
alter their behaviour according to their individual circumstances, it
is not surprising that a Google Scholar search for "
preterm birth" and "vitamin D" turns up articles confirming the benefits of higher 25-hydroxyvitamin D. For instance, from
Carol Wagner et al. 2014:
25(OH)D values closer to delivery were more strongly correlated with gestational age at delivery than earlier values
At baseline, those who had serum concentrations <50 nmol/L (20 ng/mL) 25-hydroxyvitamin D had 3.3 times of odds of a preterm birth compared to those with serum concentrations ≥100 nmol/L (40 ng/mL; p = 0.27).
At 2nd trimester, the odds were 2.0 fold (p = 0.21) and at the end of pregnancy, the odds were 3.8 fold (p = 0.01).
Likewise,
Autism Spectrum Disorder - at least among some population groups. From
Lee et al. 2019, regarding the Stockholm Youth Cohort:
Maternal 25-hydroxyvitamin D was not associated with child ASD in the overall sample.
However, in Nordic-born mothers, maternal 25OHD insufficiency
(10 to < 20 ng/mL) at ~11 weeks gestation was associated with 1.58
times higher odds of ASD (95% CI: 1.00, 2.49) as compared with 25-hydroxyvitamin D
sufficiency (≥20 ng/mL).
Neonatal 25-hydroxyvitamin D < 10 ng/mL was associated
with 1.33 times higher odds of ASD (95% CI: 1.02, 1.75) as compared with
25-hydroxyvitamin D ≥ 20 ng/mL.
Our results are
consistent with an increasing body of evidence suggesting that vitamin D
concentrations in early life may be associated with increased risk of
neurodevelopmental disorders including ASD [Autism Spectrum Disorder].
From
Sourander et al. 2021,
who split their 25-hydroxyvitamin D distribution into five quintiles,
here in ng/mL: < 8, 8 - 16, 16 - 24, 24 - 32 and > 32.
Analyses by quintiles of maternal
25(OH)D levels revealed increased odds for ASD in the 2 lowest
quintiles, <20 ng/mL aOR [adjusted odds ratio] 1.36, 95% CI [confidence interval WP] 1.03–1.79, p = .02 [statistical significance WP]) and 20–39
ng/mL (aOR 1.31, 95% CI 1.01–1.70, p = .04), compared with the highest
quintile. The increased risk of ASD was observed in association with
deficient (<12 ng/mL) (aOR 1.44, 95% CI 1.15–1.81, p = .001) and
insufficient (12 - 20 ng/mL) maternal 25(OH)D levels (aOR 1.26, 95% CI
1.04–1.52, p = .01) compared with sufficient (≥20 ng/mL)
levels.
I do not recall any research based on
50 ng/mL 25-hydroxyvitamin D being regarded as "sufficient", "adequate",
"necessary for good health" - which is the clear impact of the Quraishi
et al 2014 research. Most researchers follow guidelines which
were developed primarily or wholly to reflect the needs of the kidneys,
in which 20 ng/mL or perhaps 30 ng/m: is regarded as "sufficient".
There is reliable evidence for low maternal and so in-utero
25-hydroxyvitamin D levels causing (or at least contributing very
strongly, to the point where if levels where higher, the condition
would not occur) autism and other neurodevelopment disorders which catastrophically disrupt the person's ability to live happily, including by contributing to the lives of others:
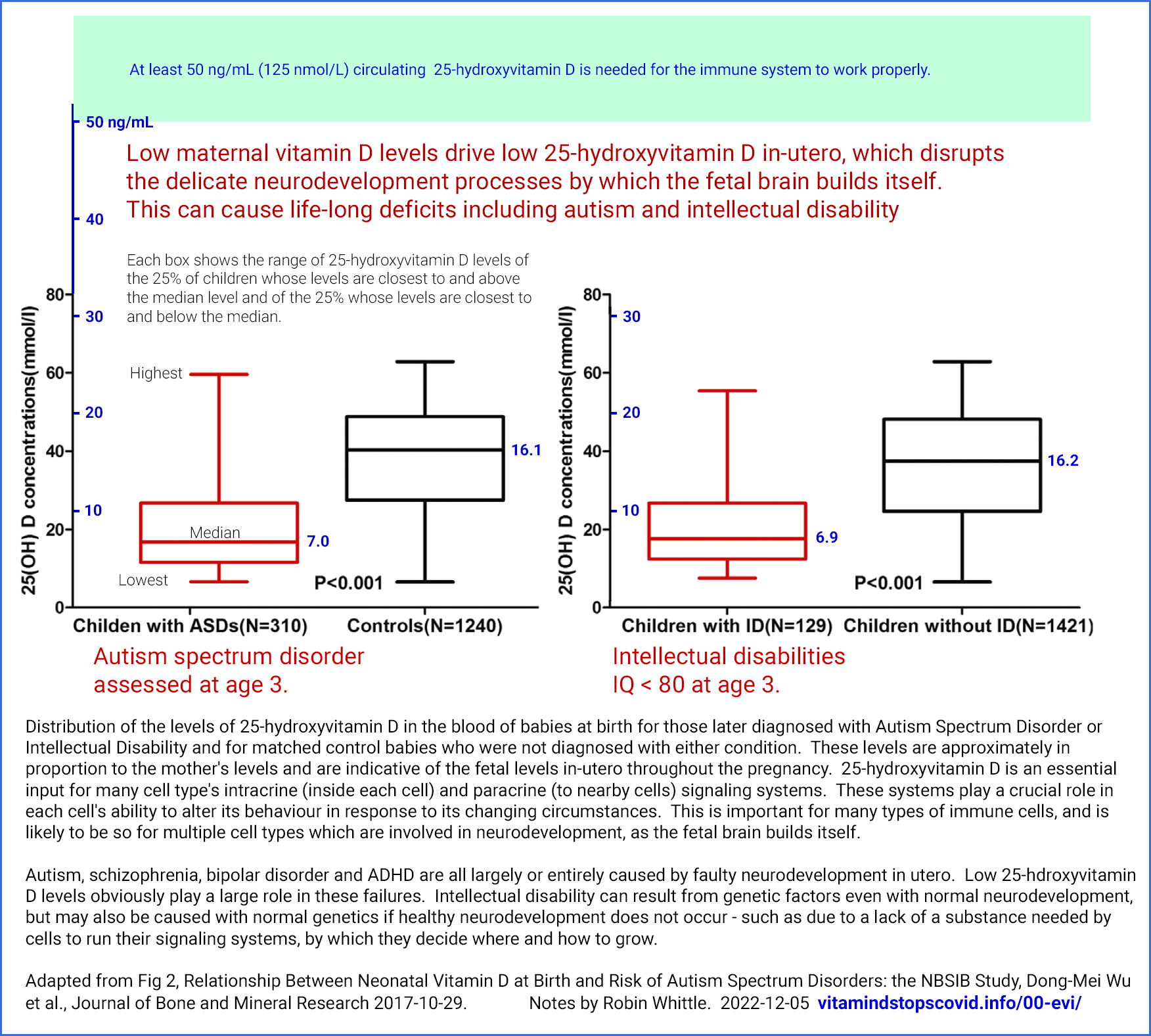
These graphs are from:
Genetic and other nutritional factors surely contribute to the
incidence of autism, intellectual disability, ADHD, schizophrenia and
bipolar disorder, but the very strong relationship with low maternal
(and so low in-utero and at birth) 25-hydroxyvitamin D shows that this
deficiency is the one most urgently in need of correction.
There can be no reverse causation from a later diagnosis of ASD (Autism
Spectrum Disorder) to in-utero (and so early childhood)
25-hydroxyvitamin D levels. A counter-argument is that the cause
was low 25-hydroxyvitamin D in the years leading up to the diagnosis,
and that in-utero levels were correlated with this, but did not
actually cause the problem. However, attempts at treating ASD
with vitamin D supplementation have produced only marginal results (
Li et al. 2020).
These are all profound, lifelong, disabilities whose cause is widely
accepted as being primarily or wholly in faulty neurodevelopment
in-utero.
It could also be argued that low 25-hydroxyvitamin D levels were merely
markers for other aspects of ill-health (poor diet, lack of other
nutrients, lack of sunshine and exercise for the mother) but were not a
significant cause of the tragic observations. However, the
strength of the association and the knowledge of, and other reasonable
assumptions about, the role of vitamin D in many cell-types' ability to
respond to their changing circumstances are very strong arguments for a
directly causative role of low 25-hydroxyvitamin D in-utero.
Low maternal 25-hydroxyvitamin D would increase rates of viral
infection, and those viruses, the immune response to them and the
raised temperatures which result (which are a healthy part of the
immune response) may also contribute to whatever disrupts the ability
of the fetus's brain to build itself, particularly in the earlier
months of pregnancy, when overall brain structures and populations of
different cell types are being laid down.
This and similar research is all the justification any person, health
organisation or government needs to pursue, with urgency and vigour,
whatever actions will increase the 25-hydroxyvitamin D levels of
all women of childbearing age.
It is not good enough to wait until pregnancy had been recognised and
then start supplementing vitamin D. That may be too late, even if
the 25-hydroxyvitamin D levels were raised in a few hours with a single
oral dose of ~1 mg of calcifediol (which
is 25-hydroxyvitamin D).
Among women of child-bearing age worldwide, several populations are at
greatest risk and should be prioritised in such campaigns:
- Women living far from the equator.
- Women who have brown or black skin.
- Women who avoid skin exposure to sunlight - particularly women in Muslim cultures.
All three of these conditions are true of millions of women. A section above
#03-uk-low
shows that even in sunny Israel, Arab (and so predominately Muslim)
women have disastrously low 25-hydroxyvitamin D levels. Far from
the equator, in the UK, graphs in that section show disastrously low
levels for most of the population with genetic and cultural backgrounds
in Africa, Pakistan, India and Bangladesh.
Prevention is always better than cure. Prevention of these
lifelong disabilities is infinitely better than cure, because there is
no cure for failures of neurodevelopment.
The following article has extensive references:
The process of development depends on a number of signaling systems that
regulates the progressive sequence of developmental events. Infertility
and neurodevelopmental diseases, such as attention deficit
hyperactivity disorder, autism spectrum disorders, and schizophrenia,
are caused by specific alterations in these signaling processes.
Calcium
signaling plays a prominent role throughout development beginning at
fertilization and continuing through early development, implantation,
and organ differentiation such as heart and brain development. Vitamin D
plays a major role in regulating these signaling processes that control
development. There is an increase in infertility and an onset of
neurodevelopmental diseases when vitamin D is deficient.
Nobles et al. 2015
studied maternal 25-hydroxyvitamin D levels at ca. 15 weeks gestation
among ethnically diverse women in (42° from the equator)
Massachusetts. They found significantly
lower birth weights when the mother's 25-hydroxyvitamin D levels were lower in the distribution. Their findings in summary:
53·2%
of mothers had <30 ng/mL 25-hydroxyvitamin D levels and 20·7% had
<20 ng/ml. Women with (adjusted) <30 ng/mL levels [I assume this includes women with < 20 ng/mL] had babies weighing 140 grams less than those born to mothers whose 25-hydroxyvitamin D levels were 30 ng/mL or more.
The average weight of babies born to mothers whose 25-hydroxyvitamin D was < 20 ng/mL was 176 grams less.
Immunologists, doctors and public health officials should be avidly
pursuing research such as this and so should be taking the strongest
possible action to bring potential mother's 25-hydroxyvitamin D levels
up, ideally to at least the 50 ng/mL needed for proper immune system
function.
With rare exception, they are not doing this. They seem far more
interested in drugs and vaccines. It seems that immunologists are
forever toiling, debating and grappling with the intrigues of
this cell-type, that cytokine and the other genetically determined
variation in structure of one of countless thousands of enzyme or
receptor molecules. All these intrigues are used to justify
funding for further research, which is fine from the point of view of
pure science. However, most such research - like much of
conventional medical practice - is wrong or at least incomplete, since
those conducting it do not understand the immune system's critical need
for a level of 25-hydroxyvitamin D which most people do not have.
It is a grave professional failing not to recognise and work to urgently eliminate an
easily
and safely correctable nutritional deficiency which condemns many
people to permanent, disastrous, physical, cognitive, emotional and
social limitations, before they were born.
There is
no need for more research
before promoting and supporting (not mandating) proper vitamin D
supplementation for all women of childbearing age, as the first step in
extending this to all people from birth to old age.
Further information on the need for improving 25-hydroxyvitamin D levels of women before they become pregnant:
vitamindwiki.com/Ensure+a+healthy+pregnancy+and+baby+-+take+Vitamin+D+before+conception
Update 2023-06-05:
This article from Finland demonstrates that children in general - or at
least some children - benefit significantly by having 0.03 mg (1200 IU)
supplemental vitamin D3 per day, more than by having 0.01 mg 400 IU per
day, for the first two years of life, as measured by psychiatric
problems at 6 to 8 years of age:
Effect
of Vitamin D3 Supplementation in the First 2 Years of Life on
Psychiatric Symptoms at Ages 6 to 8 Years A Randomized Clinical Trial
Samuel
Sandboge, Katri
Räikkönen, Marius Lahti-Pulkkinen, Helena Hauta-alus, Elisa
Holmlund-Suila, Polina Girchenko, Eero Kajantie, Outi Mäkitie, Sture
Andersson and Kati Heinonen
JAMA Pediatrics
2023-05-19
jamanetwork.com/journals/jamanetworkopen/fullarticle/2805032
The mothers - and so the newborns - had better 25-hydroxyvitamin D
levels than would be found in most Western countries, presumably due to
better supplementation and to some extend due to greater consumption of
fatty fish and/or vitamin D fortified food.
The 0.01 mg 400 IU / day children averaged 35.5 ng/mL circulating
25-hydroxyvitamin D, which is a lot higher than would be attained by
most children in most countries without post-natal vitamin D3
supplementation. The 0.03 mg 1200 IU / day children were taking about
three times the vitamin D3 per day most governments recommend, and
attained an average 48.1 ng/mL circulating 25-hydroxyvitamin D level -
which is an good outcome.
The 1200 IU group had half the "internalizing" clinically significant
problems at follow-up (p = 0.4). Intriguingly, 4.6% of their parents
were single at follow-up, compared to 11% for the 400 IU group (p =
0.04). This suggests that the child's good health, likely in many more
aspects than were measured in this trial, significantly improved the
chances of their parents remaining together.
This two year intervention showed significant benefits at the higher
intake compared to the lower, in the psychiatric attributes which were
assessed. It is easy to imagine that other benefits ensued and that
all benefits would have ensued more with continued supplementation
after two years. Likewise with proper vitamin D3 supplementation of
the mothers before and during pregnancy to ensure they all had at least
50 ng/mL (125 nmol/L) circulating 25-hydroxyvitamin D, to give their baby
the best chance of building its body and brain, in the whole of the
pregnancy.
It is possible that further benefits would have occurred with higher
intakes. However, at some level - likely different for each child in
ways which cannot be known with certainty - higher levels still would
produce no further benefits and/or significant ill effects. Note that
just under half the children in the 1200 IU / day group attained what
we reasonably assume is the 50 ng/mL (125 nmol/L) 25-hydroxyvitamin D
level at and above which the immune system is likely to work optimally.
3.3 Parkinson's disease and other forms of neurodegeneration
This section added on 2022-12-05.
It contains some key points from a much longer page, which is not yet
finalised or public, on Parkinson's disease, dementia with Lewy bodies
and multiple system atrophy. Please contact me
(rw@firstpr.com.au) if you have a special interest in these.
The etiology of Parkinson's Disease is widely regarded as being poorly
understood. The disease itself - involving the destruction of
neurons which release dopamine, in the substantia nigra - is
universally regarded as incurable. Treatment involves attempts to
minimise the severity of symptoms. Disease progression involves
diminishing ability to control the limbs, dementia and death.
These three neurodegenerative diseases are closely related, since they
all involve the misfolding of the alpha-synuclein protein, which has
important roles in several types of brain cell. Once folded in a
particular shape, the folded protein is able to catalyse the same
pattern of misfolding in another such protein, which sticks to the
first one, forming a plaque, inside cells. This somewhat
resembles three different patterns of crystallisation.
- Parkinson's Disease (PD) [WP]
affects
about 1% of people over 60.
- Dementia with Lewy Bodies (DLB) [WP] affects
about 0.4% of people older
than 65.
- A rare PD-like neurodegenerative disease Multiple System Atrophy
(MSA) [WP] affects about 0.005% of people.
In:
Different α-synuclein prion
strains cause dementia with Lewy bodies and multiple system
atrophy
Jacob I. Ayers, Joanne Lee, Amanda L. Woerman, Ann A.
Lazar, Carlo Condello, Nick A. Paras, and Stanley B. Prusiner.
PNAS Neuroscience 2022-02-03
www.pnas.org/doi/abs/10.1073/pnas.2113489119
the researchers used a variety of subtle in-vitro (cell culture in
test tubes) techniques to show that the precise misfolded
structures of alpha-synuclein in Parkinson's disease, dementia with
Lewy bodies and Multiple System Atrophy, while unknown, were all
different.
Excessive inflammation is well known to be involved in these and
numerous other neurodegenerative diseases which involve protein
misfolding. "Amyloid" refers to these misfolded states.
There's a long list of these diseases at:
Amyloid diseases are a subset of prion diseases
en.wikipedia.org/wiki/Prion,
which are considered incurable, since no-one (so most people think) has
a way of slowing or halting the agglomeration. Two well-known
prion diseases are "Mad cow disease" and the closely related
Creutzfeldt-Jakob disease [
WP]. These
can
start spontaneously - a single or two molecules of the protein folding
in the particular prion pattern, and then other molecules folding
according to this pattern and so joining the agglomeration.
Here we are concerned with common neurodegenerative diseases, the
conditions which favour their development and what might be done to
reduce or prevent this. While the focus is on PD, much of what
applies to it, regarding underlying etiology and how the disease might
be prevented, or slowed once it starts, also applies to Alzheimer's
disease and many other forms of neurodegeneration in old age.
Upon using Google Scholar to research PD and MSA, it took me about three minutes to find this highly significant article:
Circulatory 25(OH)D and
1,25(OH)2D as differential biomarkers between multiple system
atrophy and Parkinson's disease patients
Hiromu
Ogura, Izzettin Hatip-Al-Khatib,
Midori Suenaga, Funda Bolukbasi Hatip, Takayasu Mishima, Shinsuke
Fujioka, Shinji Ouma, Yoichi Matsunaga and Yoshio Tsuboi.
eNeurologicalSci
2021-09-17
www.sciencedirect.com/science/article/pii/S2405650221000617
Ogura et al.'s observations about circulating
25-hydroxyvitamin D are of the utmost significance. The healthy controls averaged
26.8 ng/mL.
Although
50 ng/mL is needed for proper immune function, this is
actually a pretty good level for ordinary people not living near the
equator and getting around for much of the day with little or no
clothing. The research was in Japan, and I attribute the 26.8 ng/mL
level - 5 or 10 ng/mL better than what I think we would fine in the
UK, Australia or the USA - as being due to the Japanese eating quite
a lot of oily fish, which contains at least some vitamin D3.
Supplementation would also have played a role.
In Table 1, "HS" means "Healthy Subjects". (They can't be fully
healthy with just 26 ng/mL 25-hydroxyvitamin D, but in this context
they are healthy, since they are aged matched people who have
neither MSA nor PD.)
HS 26.85 +/- 7.62
MSA 10.53 +/- 3.82 (p = 0.0001)
PD 13.36 +/- 4.76 (p =
0.0001)
Readers who have read lots of research articles probably gasp at
these figures. MSA is a supposedly incurable disease (as are PD and DLB)
in which sufferers average
60.8% lower circulating
25-hydroxyvitamin D than age-matched controls.
This is a drastic difference, especially considering the second figures,
which are (I assume) the standard deviation [
WP] of
the levels observed. If the levels exhibited a reasonably
bell-curve-like "normal" distribution, then about 68% of the HS
people's levels would be within the range specified by "+/- 7.62": 19.23 to 34.47 ng/mL.
Only 2.2% of these levels would have fallen two standard deviations
below the mean - below 11.61 ng/mL. Yet more than half of the MSA
sufferers have 25-hydroxyvitamin D levels below this.
The third figure is the statistical significance [
WP]. "p = 0.0001" means that if
there were, in fact, no underlying relationship between MSA and
25-hydroxyvitamin D levels, then in the samples of the size used in
this study, with their particular distributions (roughly described by
the standard deviations) then, due to random variation, a research
study with this deviation would only occur once in every 10,000 or more
studies.
Most scientific articles adopt p < 0.05 (one in 20 chance of the
deviation occurring due solely to chance) as being "significant". So
these MSA and PD deviations are statistically
highly significant.
Here is the graph of these figures, with a more detailed representation
of the distribution of values, with the tops and bottoms of the boxes
denoting the 1/4 (quartile) of subjects with levels immediately above
and below the median, represented by the line in the middle of the
box. The upper and lower bars represent the top and bottom of the
range of all observations. The X represents the mean.
One could argue for reverse causation - people suffering from PD or MSA
don't go out in the sun as much as those who don't. However, this
article:
High Prevalence of
Hypovitaminosis D Status in Patients With Early Parkinson
Disease
Marian L. Evatt et al.
JAMA Neurology 2011-03-??
jamanetwork.com/journals/jamaneurology/fullarticle/802599
(Paywalled PDF.)
sci-hub.se/10.1001/archneurol.2011.30
reports zero or perhaps only a very
slight degree of reverse causation:
Vitamin D concentrations
did not decline during progression of PD.
If the clinical and research aspects of medicine were working
properly,
Ogura et al. - now just a year old - would have been
trumpeted in the mainstream media and in research journals and
medical conferences as being very strong evidence that the
progression of MSA and PD could be reduced, and perhaps stopped,
simply by the use of vitamin D3 supplements.
However, the whole system is broken in ways which are too complex
and distressing to discuss here. On 2022-12-05,
Ogura et al. has been
cited 5 times. Only two of these are by other teams and not involving a poison induced rat model of PD.
Here is direct, incontrovertible, evidence that vitamin
D supplementation slows the progression of PD:
Randomized, double-blind,
placebo-controlled trial of vitamin D supplementation in
Parkinson disease
Masahiko Suzuki, Masayuki Yoshioka, Masaya Hashimoto,
Maiko Murakami, Miki Noya, Daisuke Takahashi, Mitsuyoshi Urashima
The American Journal of Clinical Nutrition 2013-03-13
ajcn.nutrition.org/article/S0002-9165(23)05507-7/
This article has been
cited
217 times in the 9 years since it was published. I have not
yet tried to survey these articles, but my impression is that it has frequently been unreasonably
dismissed.
Suzuki et al.'s RCT involved Japanese PD patients, with baseline
25-hydroxyvitamin D levels of about 22 ng/mL. The intervention
group received 0.03 mg 1200 IU of vitamin D3 a day, for
12 months,
with compliance estimated as 89%. This is a fraction of what is
required to get most people's level above 50 ng/mL, at the end of
the 12 months, the intervention group's mean 25-hydroxyvitamin D
level was 41.7 ng/mL from baseline 22.5. The placebo group's mean
level was 21.4 ng/mL from baseline 21.1.
The mean disease duration at the start of the RCT was 24 months for the
vitamin D group and 13 months for the placebo group. (I don't
know how this would affect their measurements of disease progression,
but I assume it was not significant, since they don't mention it.)
Some of their observations concern differences in disease progression which
correlated with particular genetic variants of the vitamin D
receptor (VDR) [
WP]
and vitamin D binding protein [
WP]
which binds to most circulating 25-hydroxyvitamin D. Here I am
concerned with their overall results. They found (3rd column of
Table 2) reasonably statistically significant (0.028 and 0.036
respectively, increases, in the vitamin D group, of the number of
patients who showed no worsening or improvement (I would have
thought no worsening on its own would be more pertinent) in two of
18 measures of disease progression: Hoehn and Yahr stages 1 - 5 [
WP]
and UPDRS part II [
WP].
13 of the 18 measures showed improvement:with an RR (Relative risk) [
WP]
greater than 1.00, meaning a greater proportion of people in the
vitamin D group did not get any worse in the 12 months
compared to those in the placebo group. I have no knowledge of
these measures, but I calculated the mean RR for all measures was
1.2. This means that on average, over all these measures, 20%
more patients who took the 1200 IU per day vitamin D had no change in
symptoms, compared to those who did not take any vitamin D.
It is reasonable to assume that if more vitamin D3 was supplemented,
higher 25-hydroxyvitamin D levels would have been reached, and
further reductions in disease progression would have been achieved.
This leads to the Coimbra protocol - raising 25-hydroxyvitamin D
very substantially over 50 ng/mL - which I discuss below.
Likewise, this Suzuki et al. 2013 article has been largely ignored.
The Coimbra Protocol, using much higher than normal amounts of
supplemental vitamin D3, is routinely used to treat a variety of
autoimmune inflammatory disorders, many or all of which can also be
treated by helminthic therapy. Please see
vitamindstopscovid.info/06-adv/
for more on helminths and high vitamin D3 intake protocols. The
people using helminths never seem to think about vitamin D, and the
people using vitamin D never seem to think about helminths, but both
techniques, on their own, seem (to me) to be effective and reasonably
safe. Neither of these two sets of techniques has yet been full
documented in the peer-reviewed research literature. I am sure
that most doctors, immunologists and rheumatologists have never
heard of them.
There are links to 113 pages, each a testimony with photographs of a person who benefited from the Coimbra protocol.
www.coimbraprotocol.com/testimonials-1
The diseases include (October 2022):
71 Multiple sclerosis
7 Rheumatoid arthritis
7 Atopic dermatitis
4 Myasthenia gravis
3 Vitiligo
3 Psoriasis
2 Neuromyelitis Optica (NMO) or Devic's disease
2 Lupus
2 Lyme disease
2 Sjogren's syndrome
1 Spongiotic dermatitis
1 Fibromyalgia
1 Alopecia
1 Schleroderma
1 Sjogren's syndrome
1 Psoriatic arthritis
1 Idiopathic thrombocytopenic purpura
1 Type 1 diabetes (
This is extraordinary.)
1 Autoimmune polyneuropathy
1 Ichtyosis
1 Crohn's disease
This forum page has two of reports from, or about, PD sufferers who found relief with the Coimbra protocol:
Two other reports:
A Facebook video of a man playing piano:
This is one of
the first patients of Dr. Coimbra, 16 years with PARKINSON'S DISEASE
and the COIMBRA PROTOCOL! André Linn's post in the group Protocolo
Coimbra - Brasil.
"To the beginners in the Coimbra Protocol for Parkinson's, I publish
here a video made today on my godfather's 80th birthday who, since
2004, when diagnosed with the pathology, has had the blessed doses of
D3. He's the pianist.
Cheers to all!"
This patient is currently taking 50,000 IU a day.
A
Facebook video of a man riding his bike.
Adriano Chagas's post:
"About 4 years ago I started with
the first symptoms of Parkinson's. And slowly the symptoms got worse.
But still I chose not to treat by conventional treatment.
I prioritized supplementation and not stop exercising, even if it got harder and harder. But faith in God was always my forte!
About 4 months ago I started with
the Coimbra protocol with Dr Claudio Urbano. It seems like a miracle!
Sometimes I feel back to normal. I'm even back to riding my bike daily!
Thank God and the protocol !! "
Further information on the Coimbra protocol and related high vitamin D treatments for a variety of diseases:
vitamindwiki.com/Many+diseases+treated+by+high-dose+Vitamin+D This includes research showing that MS is more prevalent away from the equator and among those with brown or black skin.
We can reasonably assume that PD (and so MSA and DLB) progression is
strongly increased by low 25-hydroxyvitamin D driven, overly
inflammatory, dysregulated, immune responses. So there is a good
theoretical basis for understanding how boosting 25-hydroxyvitamin D
levels could reduce or halt disease progression. That would be an
immense blessing to the millions of people who suffer from these
diseases.
These reports of success against PD go further. The patients
recovered
some previously lost motor control abilities. This implies that,
at least in some circumstances, the brain is able to recover
functionality by either growing new neurons to replace those which have
been destroyed, or perhaps by recruiting other, already existing,
neurons, to take over their roles.
On this basis I am sure that Parkinson's disease
is
curable in some or perhaps many cases - and that at least we can expect
a reduction or cessation of disease progression with higher than 50
ng/mL 25-hydroxyvitamin D and/or with helminthic therapy.
Further information on vitamin D and Parkinson's disease:
vitamindwiki.com/Parkinson.
#04-health
4 The need for 50 ng/mL (125 nmol/L) 25-hydroxyvitamin D
There is a vast research literature on
vitamin D. Not all of it is particularly interesting - there are
too many low-key review articles which add little to our knowledge and
which may perpetuate falsehoods, such as "vitamin D is a secosteroid
hormone", or which discuss immune system function without clearly
identifying the non-hormonal vitamin D based intracrine and paracrine
signaling mechanisms which immune cells rely on.
You can use Google Scholar to search for research articles on the
relationship between observed or experimentally altered
25-hydroxyvitamin D levels and health outcomes:
These are a few of dozens of major health problems whose incidence
and/or severity are worsened by 25(OH)D levels significantly below 50 ng/mL (125
nmol/L). The best of these research items are linked to
from the left column at vitamin D researcher Henry Lahore's
vitamindwiki.com.
For brevity, this section mentions only a small subset of the relevant research.
4.1 Seasonality and so incidence and severity of influenza
The
seasonality of influenza and other viral respiratory diseases
has long been known. Though this is often attributed to
variations in outdoors temperature and humidity, and to a people
spending more time indoors in winter (where most transmission occurs),
these mechanisms explain only a small part of the seasonal
variations. Indoor and in-vehicle temperatures rise and
humidity falls in winter - the opposite to the seasonal changes in
outdoor conditions.
The best explanation for this seasonality, in countries far from the
equator, is the change in average 25-hydroxyvitamin D levels.
Higher 25(OH)D levels in summer and autumn enable better innate and
adaptive responses to all kinds of pathogens. This improved
immune system competency has at least three effects in whole
populations:
- Reduced chance of becoming infected for any given viral insult.
- Reduced severity of symptoms for those infected - including increased chance of no symptoms at all.
- Reduced community-wide rates of transmission due to lower average levels of viral shedding by those who are infected.
The first mechanism is important, but the other two are still more
significant. The second affects perceived levels of infection and
the level of suffering, harm and death for those who are
infected. The third strongly attenuates average rates of
transmission and so can prevent pandemic transmission and greatly
reduce the number of people who become infected.
The following diagram is based on one originally published in:
This is from:
Epidemic influenza and vitamin D
J. J.
Cannell, R. Vieth, J. C. Umhau, M. F. Holick, W. B. Grant, S. Madronich, C. F. Garland and E. Giovannucci
Epidemiology and Infection 2006-09-07
doi.org/10.1017/S0950268806007175
Vitamin D supplementation should stabilize 25(OH)D concentrations
consistent with levels obtained by natural summertime sun exposure (50
ng/mL) while avoiding toxic levels. Those with large amounts of melanin
in their skin, the obese, those who avoid the sun, and the aged may need
up to 5000 IU/day to obtain such levels, especially in the winter.
Cannell et al. also wrote that the hypothesis should be tested:
Are patients with low 25(OH)D levels more likely to contract viral respiratory infections?
This call was answered by:
who reported on a beautifully designed, 3 year long, double-blind [
WP], placebo-controlled [
WP] RCT (randomised controlled trial [
WP]) involving 208 post-menopausal African American women in Long Island, New York State, USA. This diagram explains the results:
In the intervention group, 0.02 mg 800 IU/day vitamin D3 resulted in 7
infections over two years (grey) with only a little more in winter,
while placebo group (black) reported 26 episodes over three years,
mostly in winter. In the third year, the same 104 women were given
0.05 mg 2000 IU/day D3 (green) and there was only one episode, in summer.
The very small supplemental intake of 800 IU/day D3 greatly reduced
influenza incidence (though asymptomatic infection would not have been
detected), and abolished the concentration of cases in winter. Just
0.05mg 2000IU/day D3 almost entirely abolished influenza for these women all year round.
This is not the same as raising the 25-hydroxyvitamin D
levels of whole populations, or of the great majority of a
population. In this trial, the subjects were living in a generally
unsupplemented community and so were at the currently normal risk of
being exposed to influenza viruses, which is much higher in winter due
to more people being infected then. This trial measured the ability of
individuals to avoid symptomatic infection in a setting of unchanged
viral insults.
If an entire population raised their 25-hydroxyvitamin D levels in
the same way as the women in the intervention group, then we would
expect still fewer infections, since all individuals would be less
likely to develop symptomatic influenza for any given viral
insult. This reduction in symptomatic cases would therefore
reduce the
average level of viral insult of all people in the population. This and
the general reduction in viral shedding by those infected would further
reduce transmission and so the total number of infections.
We
don’t know the 25-hydroxyvitamin D levels of these women. However, it
is reasonable to assume that the placebo group’s levels were around 10
to 15 ng/mL (25 to 37.5 nmol/L) and that intervention group’s levels averaged around 22 ng/mL (55 nmol/L)
for the first two years (800 IU/day) and around 38 ng/mL (95 nmol/L) for the third
year with 2000 IU/day. These are my guesstimates based on the following
graph from
Gallagher et al 2014: which
depicts the 25-hydroxyvitamin D levels for five groups of African
American women who were given zero, 0.01mg 400IU, 0.02mg 800IU, 0.04mg
1600IU and 0.06mg 2400IU D3 a day for 12 months.
As an aside, the above data shows that:
- The UK government's currently recommended vitamin D
supplementation quantity of 0.01 mg 400 IU only raises 25(OH)D levels a
small fraction of what they need to be raised in order to attain 50
ng/mL (125 nmol/L).
- Daily intakes of 4 and 6 times this amount (1600 and 2400 IU) do not raise average
levels 4 or 6 times as much. This shows that 25(OH)D levels
are not proportional to vitamin D3 intake levels. The self-limiting
mechanism makes it harder and harder to raise the level as the level
gets higher. See the Heaney et al. 2015 and Ekwaru et al. 2014 graphs in a section below: #05-history
4.2 Seasonality and severity of COVID-19 and influenza
An important foundation of the
following sub-section is that in COVID-19, the degree of viral shedding
scales with disease severity. This is reasonable to expect of any
viral disease, and it is confirmed by the following observations by
Wang et al. 2020
www.jci.org/articles/view/138759 :
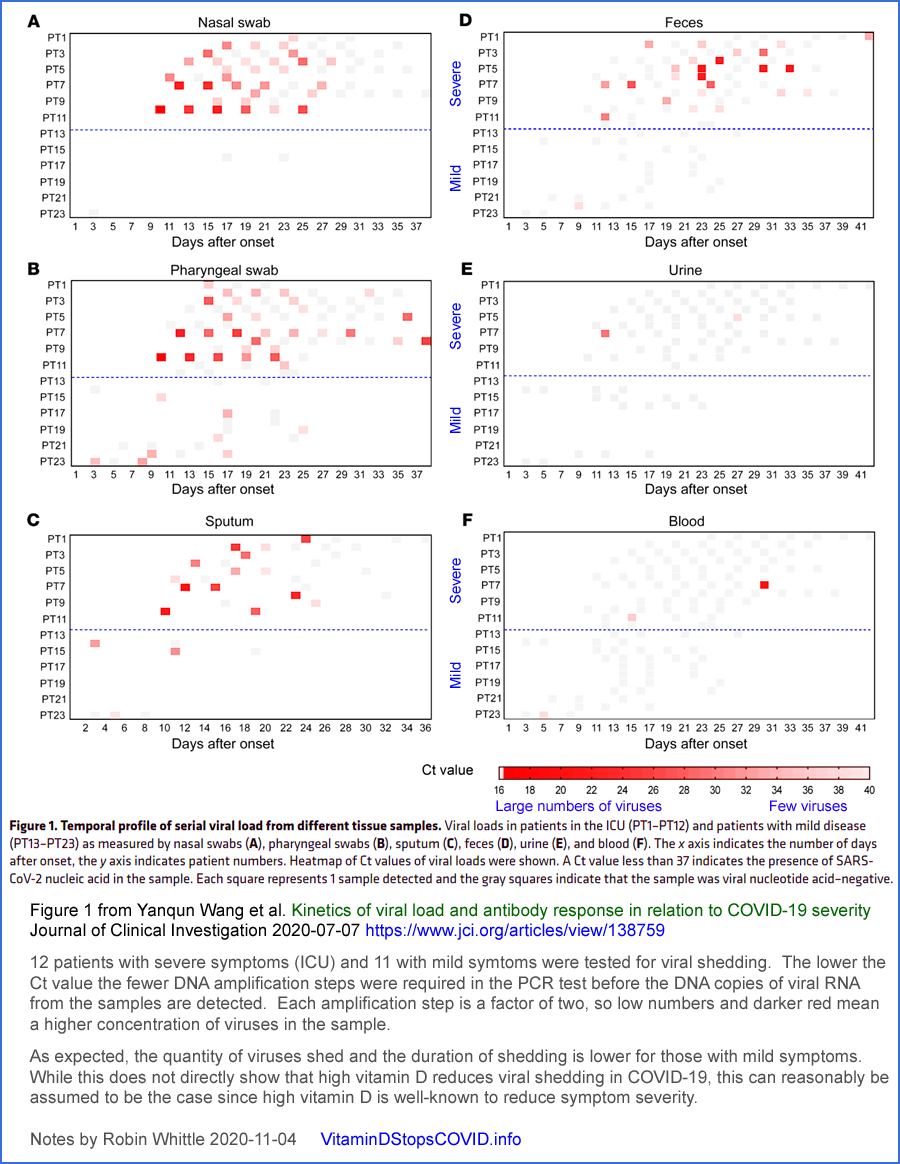
While new, more highly infectious
variants in 2021, especially those of the Omicron clade, produced
rapidly changing levels of COVID-19 infection, harm and death, a
seasonal component to COVID-19 transmission is still evident.
It follows from all we know about:
- The immune system's dependence on good 25-hydroxyvitamin D levels.
- The variation of population average and individual
25-hydroxyvitamin D levels with the season, due to varying levels of
UV-B skin exposure.
- The observed inverse relationship between 25-hydroxyvitamin D levels and COVID-19 severity. Please see
the graph several pages below showing this relationship, from Vanegas-Cedillo
and other research articles: #4.4
- Viral shedding increasing according to disease severity.
that COVID-19 transmission, case numbers and the harm and death which
results should follow a seasonal pattern like that of influenza.
The following chart depicts this seasonality in action in the UK in the summer of 2020.
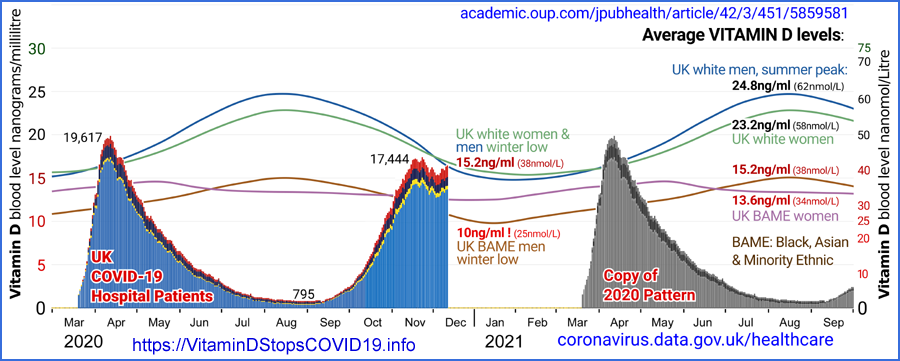
I made this in December 2020 with carefully matched BIOBANK monthly 25(OH)D graphs derived
directly (not manually copied) from Raisi-Estrabragh et al. 2020
doi.org/10.1093/pubmed/fdaa095 and the hospitalised patients graph from
coronavirus.data.gov.uk/details/healthcare.
The right side is my attempt to predict hospitalised patient numbers in
2021. The hospital patient numbers in blue are all due to the original variant of
SARS-CoV-2. B.1.1.7, later known as Alpha, only became
significant in the UK in December 2020 [
WP].
The graph in blue represents a dramatic seasonal variation in the
transmission and severity of the original (in the UK at least)
SARS-CoV-2 variant. This was before the introduction of mRNA and adenovirus vector
quasi-vaccines directed at COVID-19. There was no early
treatment. In the summer of 2020, there were no lockdowns and -
as far as I know, little social distancing or adoption of masks.
Something about the UK 2020 summer reduced R0 [
WP]
to well below 1.0, so the virus was not spreading as an epidemic.
If the August 2020 conditions had remained, COVID-19 would have largely
or entirely died out in the UK by the end of the year.
We don't know the actual 25(OH)D levels of even a representative sample
of UK citizens in the summer of 2020. The BIOBANK graphs
give a general indication of seasonal trends.
These 25(OH)D variations, although never approaching what is truly
adequate for immune system health, nonetheless are highly significant
summer improvements on the lower levels which resulted from limited UV-B exposure in winter and spring.
While the summer solstice at June 21 is the theoretical peak of UV-B
availability in the northern hemisphere, actual skin exposure depends
also on warmer temperatures, which lag the solstice by a month or two
due to the thermal inertia of the oceans. (The lag is a little
longer in the southern hemisphere, which has more ocean). Warm
temperatures drive more bare skin around midday and so more vitamin D3
for a significant proportion of the population. The liver takes a
few days to convert it (actually only about 1/4 is converted) to
circulating 25-hydroxyvitamin D and this has a half-life, at these
still low levels (compared to 125 nmol/L), of a month or so.
The marginal reduction of time spent in buildings in summer cannot
explain more than a small fraction of this drastic attenuation in
SARS-CoV-2 transmission. Time spent in vehicles, public and
private, would hardly change. There is surely more intermingling
between families outdoors in summer than in winter. Direct UV-B
inactivation of viruses in aerosols and on surfaces (fomites) may
explain some reduction in transmission, but this is only during the day
and only outside buildings and vehicles, since UV-B does not penetrate
glass.
The only explanation for the great majority of this life-saving
reduction in transmission and severity is the population-wide seasonal
boost in 25-hydroxyvitamin D levels.
This justifies the
Vitamin D Stops COVID name of this website.
To what extent these seasonal variations would prevent pandemic
transmission of the much more infectious Omicron variants cannot be
implied from these 2020 observations.
However, Patrick W. Chambers MD and I are advocating that everyone raise their 25(OH)D levels to 50 ng/mL (125 nmol/L) or more,
all year round.
Since even half this level was putting a stop to the original SARS-CoV-2 variant,
there's a good chance it would strongly attenuate transmission of
Omicron and future variants to the point of R0 being below 1.0, so
there would be no pandemic transmission and so an overall low number of
cases.
There have been many academic journal articles concerning
seasonality of COVID-19. These are necessarily speculative since
we can't experimentally change the seasons. Most of these
articles ignore seasonal variations in 25-hydroxyvitamin D levels and
focus on outdoors temperature and humidity and related behavioural
changes, with conflicting theories and observations. A partial survey of this literature can be found
in my Substack article:
nutritionmatters.substack.com/p/covid-19-seasonality-is-primarily .
From that article, here are some further arguments for proper
community-wide vitamin D3 supplementation to defeat the ability of
influenza,
COVID-19 and other such diseases to spread rapidly at any time of year,
and to reduce the harm suffered by those who do contract them.
Even without any knowledge of the mechanisms
by which 25-hydroxyvitamin D levels affect disease severity or viral
shedding, we can reason that in countries far from the equator:
1 - Seasonal variations in UV-B skin exposure lead to higher levels
of 25-hydroxyvitamin D in summer-autumn and lower levels in
winter-spring.
2 - Low 25-hydroxyvitamin D levels increase disease symptom severity - especially in influenza and COVID-19.
3 - Viral shedding is reasonably expected to scale with symptom severity. Wang et al. 2020’s observations confirm this.
4 - Since the quantity of viral shedding varies so much, and is a
crucial determinant of transmissibility, we can reliably conclude that
winter-spring seasonal variations in 25-hydroxyvitamin D, in the absence of robust vitamin D3 supplementation to attain high levels all year round, is a strong driver of transmissibility.
5 - Since transmissibility, for any given level of innate and adaptive immunity
in all the individuals in a population, is the primary determinant of
how many people are infected in a given time period, we can reliably
conclude that, in the absence of robust vitamin D3 supplementation to attain high levels all year round,
winter-spring seasonal variations in 25-hydroxyvitamin D levels play a
very large role in the total number of people who become infected.
6 - Once infected, disease severity - and so the overall rates of
suffering, harm and death - are strongly affected by the effectiveness
of any early or late treatments, the most important of which, in the absence of robust vitamin D3 supplementation to attain high levels all year round,
is rapid boosting of 25-hydroxyvitamin D above typically low levels
such as 5 to 25 ng/mL (12.5 to 37.5 nmol/L) to at least the 50 ng/mL
(125 nmol/L) level the immune system needs to function properly. nutritionmatters.substack.com/p/calcifediol-to-boost-25-hydroxyvitamin See also Castillo et al. 2020 below #castillo-2.
7 - In the long term, over years and decades, the harm caused by
infectious diseases is reduced to the extent that adaptive immune
responses to prior infections provide lasting protection against the
same or similar pathogens. Higher 25-hydroxyvitamin D levels, by
increasing immune system competency, provides better such protection to each
individual than is possible if they have low 25-hydroxyvitamin D levels.
8 - To the extent which most or all people in a population properly
supplement vitamin D3 to attain at least 50 ng/mL (125 nmol/L)
25-hydroxyvitamin D levels, multiple benefits ensue regarding
infectious diseases such as influenza and COVID-19, including:
Somewhat reduced chance of being infected for any given viral insult, depending on prior immunity.
If
infected, reduced disease severity, which reduces harm and the risk of
death and increased chance that there will be few or no symptoms.
If
infected, reduced viral shedding, which benefits all those currently
uninfected by reducing the rate of transmission. Ideally this results
in R0 [WP] below 1.0 so any outbreaks of infection tend to die out.
If
infected, each individual’s long-term immunity is strengthened
regarding the specific pathogen and variants of the one which caused
the initial infection.
-
With highly infectious diseases
in which sterilising immunity (which completely prevents infection)
does not last a lifetime, and which may fade over periods such as
months or a few years - as is the case for influenza and COVID-19 -
all-year-round high 25-hydroxyvitamin D levels will ensure good immune
system competency and prevent the seasonal development of the generally
low community immune competency which enables the winter-spring
seasonal epidemic outbreaks which currently drive most influenza
infection.
(The same pattern of winter-spring
seasonality would be more clearly observed with COVID-19 if its
variants settled down into changes which avoid pre-existing immunity to
some degree without drastically increasing transmissibility. The recent
rapid increases in transmissibility with Alpha, Delta and now
especially Omicron variants and sub-variants has created new infection
waves even at times of seasonally somewhat elevated 25-hydroxyvitamin D
levels.)
-
While we can’t be sure that any given level of
25-hydroxyvitamin D and availability of early treatments will thwart
epidemic transmission of future SARS-CoV-2 variants, it is obvious that
we should do all we can to boost 25-hydroxyvitamin D levels since this
is the simplest, safest, least expensive measure we can take to protect
against this and numerous other diseases.
The response by most governments and
many doctors to influenza and COVID-19 has always been wrong. It
would always have been better to boost 25-hydroxyvitamin D levels
community-wide with proper vitamin D3 supplementation than to widely
deploy vaccines.
It makes no proper sense to vaccinate individuals (which is expensive,
invasive and in the case of COVID-19, risky) when their immune systems
are not functioning due to an easily correctable nutritional deficiency.
However, this is what has been done with influenza, and now COVID-19
(with poor results in both cases, regarding transmission and protection
from severe disease), due to a number of pernicious factors.
First among these is the profitability of vaccines, which drives their
promotion.
Second is the widespread attraction many people have
to a specific, narrowly targeted, intervention - when simple, broad,
nutritional support would be more effective.
Thirdly, it seems
that for some COVID-19 vaccines or at least for some people, popular
notions of such vaccines protecting against
severe disease are not supported by all available evidence to the
degree to which they has been promised by authorities.
(2022-06-05
explanatory note not in the actual submission: The excessive faith in
COVID-19 vaccines caused some or many people to believe that they did
not need early treatment or nutritional improvement and/or that such
measures were ineffective and/or that promotion or acceptance of such
measures would reduce the uptake of vaccines, which they believed was
the only viable way of protecting the whole community. This reduced
many people's ability to benefit from such nutritional and early
treatment approaches.)
Please see the research articles cited in my two recent articles which
show that the best available observations indicate that influenza
vaccines, over many years, do not reduce hospitalisation or death for
influenza or similar diseases to any discernible degree:
While vaccine efficacy is not directly pertinent to this Call for
Evidence, it is important to note that widely held beliefs about
vaccines being the best or only way to tackle some diseases are not
supported by the best available research. Proper vitamin D
supplementation is a much better approach, though it is not promoted by
anyone, since no one will make much money from it.
The government's responsibility is to find the best solutions,
irrespective of their profitability and the degree to which they are
promoted.
4.3 High levels of infection, harm and death among BAME medical staff in the UK
One notorious aspect of the initial
COVID-19 wave of 2020 was that 90% of UK doctors who were killed were
from "ethnic minorities". The Daily Mail reports on 2020-06-13:
From this article, here are photos of some of the 300 healthcare staff who have died so far:
These people generally have even lower vitamin D levels than the poor
average of Caucasians in the UK. The deaths of doctors can't
be blamed on them living in poverty, or in overcrowded
conditions.
The widespread ignorance of the importance of vitamin D for the immune
system, and the absence of any early treatment - or even vitamin D
repletion and effective treatment in hospital - condemned these people
to serious harm and death. They were surely highly exposed to the
virus while working long hours protecting others.
Even if these people had followed UK government advice and taken 0.01
mg 400 IU of vitamin D3 a day, all year round, their 25-hydroxyvitamin
D levels would still generally have been half or less of the 50 ng/mL (125 nmol/L) their immune systems need to work properly.
4.4 Observations of 25-hydroxyvitamin D levels and COVID-19 severity
There is a plethora of research
articles on this topic. I stopped adding them to my diagram
because it was getting too cluttered. Here are a few:
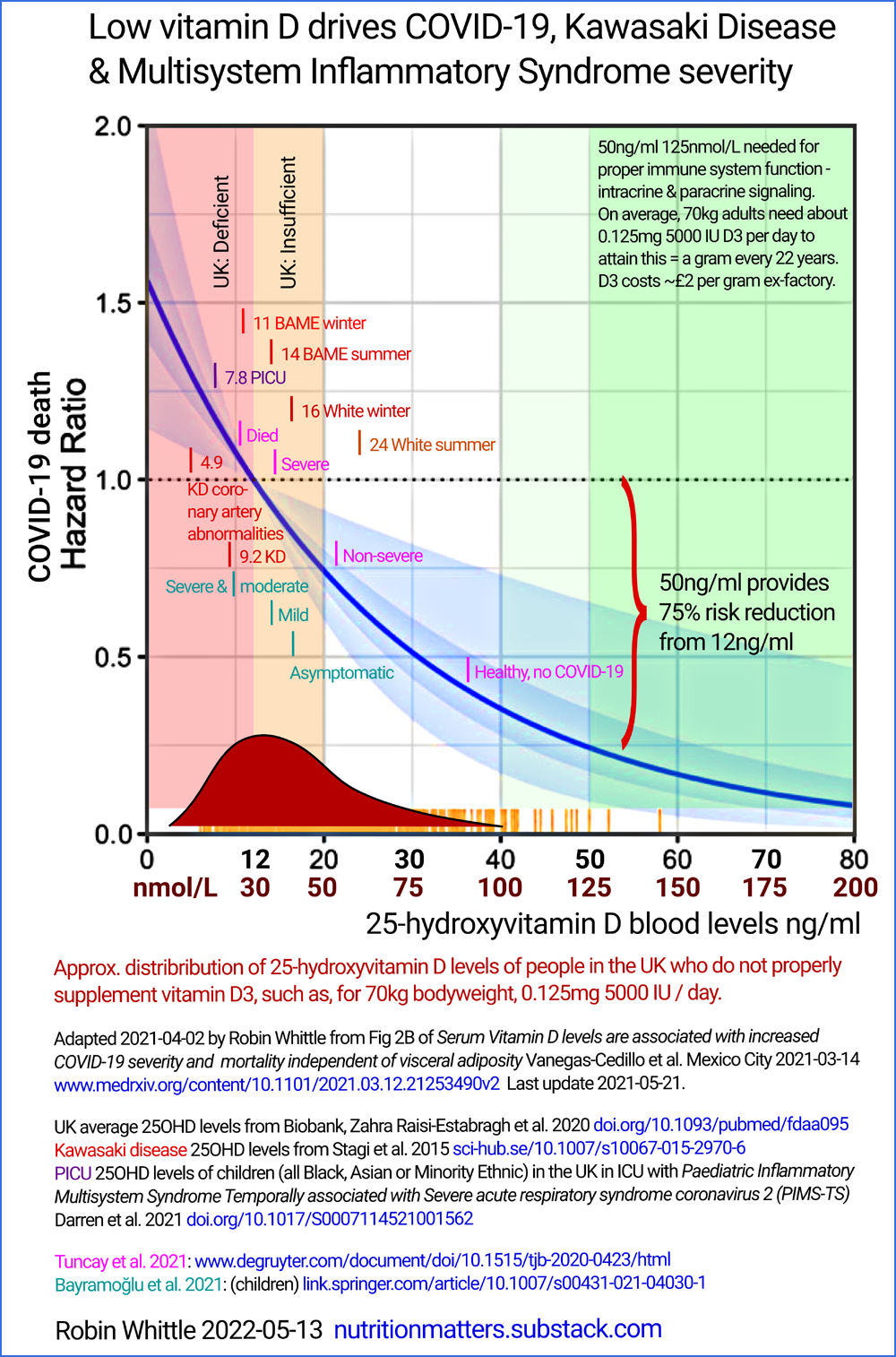
Serum
Vitamin D levels are associated with increased COVID-19
severity and mortality independent of visceral adiposity
Vanegas-Cedillo et al. Mexico City 2021-03-14
Biobank:
#2020-UK-vit-D-BAME
.
Vitamin D status of children with Paediatric
Inflammatory Multisystem Syndrome Temporally associated with Severe
acute respiratory syndrome coronavirus 2 (PIMS-TS)
Angeline
Darren, Suma Uday, Deepthi
Jyothish and 9 others
British Journal of Nutrition, 2021-05-12
doi.org/10.1017/S0007114521001562
The association between vitamin D levels
and the clinical severity and inflammation markers in
pediatric COVID-19 patients: single-center experience from a
pandemic hospital
Elvan Bayramoglu, Gülsen Akkoç, Ayse Agbas, Özlem Akgün,
Kamer Yurdakul, Hatice Nilgün Selçuk Duru & Murat Elevli
European Journal of Pediatrics 2021-03-31
link.springer.com/article/10.1007/s00431-021-04030-1
For the Stagi et al. 2015 article on Kawasaki disease see the next sub-section.
4.5 Kawasaki disease - and so Multisystem Inflammatory Syndrome AKA PIMS / PIMS-TS
Kawasaki disease (KD) [
WP] is an acute
inflammatory condition in children, mainly under 5 years, which is
triggered by a variety of viral and bacterial infections, though
sometimes the triggering condition is not known. KD was first
described in 1967 and it is a travesty that most doctors to this day
have no idea that low 25-hydroxyvitamin D is a crucial, easily
correctable, part of its etiology.
There are dozens of chronic and acute inflammatory autoimmune
diseases [
GS
Google Scholar, 1,950,000 articles]. The primary cause of these
is probably that our
inflammatory responses - which are indiscriminate cell-destroying
responses primarily directed at multicellular parasites - have evolved
over tens of millions of years to be stronger than they should
be. This is because helminths (intestinal worms), which
ubiquitously infected humans until about a century ago, long ago
evolved the ability to exude compounds which downmodulate the
inflammatory
immune responses which threaten their survival.
Human immune systems evolved to be excessively inflammatory so that
they were still reasonably effective in the presence of helminthic
downmodulation. Now, without helminths, our inflammatory immune
responses are prone to being excessively strong, which means that once
triggered, they can destroy our own cells to the extent of causing
lasting harm or death. The degree to which this occurs varies
considerably according to each individual's particular genes.
Two such compounds are currently known, but none are available as
medicines to downmodulate our immune responses in the absence of
helminths. There are good reasons we eradicated these parasites.
However, some of them are relatively benign and the benefits they
confer to some people with severe autoimmune disease, such as asthma,
rheumatoid arthritis, psoriasis etc. mean that some people deliberately
infect themselves with helminths to suppress their symptoms:
https://helminthictherapywiki.org . For more information on this, please see the research articles cited at:
Low 25-hydroxyvitamin D greatly exacerbates this problem because:
- The resulting immune system weakness results in worse
bacterial, viral and fungal infections in general, leading to a greater
chance of triggering a self-destructive hyper-inflammatory response.
- The lack of 25-hydroxyvitamin D to supply the intracrine and
paracrine signaling systems of immune cells such as Th1 regulatory lymphocytes leads to impaired
regulation of inflammatory responses. See Chauss et al. 2021 above #chauss.
Very few doctors or even vitamin D researchers are aware of the
problems caused by lack of helminths. See the above web page for
Wolday et al. 2021 who report that helminthic infection attenuates the
severity of COVID-19. The helminth researchers do not seem
to know about vitamin D and the immune system. Many doctors and
researchers working on inflammatory disorders have no idea about either
vitamin D or lack of helminths.
MIS-C, PIMS and PIMS-TS are synonyms for inflammatory conditions which
resemble KD in many ways, but these terms are usually used for
diagnosis of older
children, teenagers and some young adults, with somewhat different
patterns of vasculitis and organ damage. We can reasonably
consider these, and KD, to be regions of a single spectrum of wildly
dysregulated inflammatory responses, triggered by a typically viral
disease.
KD is known to affect children more in winter, to be more likely to
affect those far from the equator. It is also well known to be more prominent
in children with dark or brown skin. What could be the
cause? Doctors regard KD's etiology as a mystery. Yet
any London cab driver knows about winter low vitamin D, and every
doctor
should know that low
25-hydroxyvitamin D leads to weakened innate and adaptive immune
responses and to higher risks of wildly dysregulated hyper-inflammatory
"cytokine storm" immune responses, which can be triggered by a variety
of conditions.
Stagi et al. looked into the matter in 2015:
The patients were 21 girls and 58 boys, average age 5.8 years.
Their average 25(OH)D levels were
9.2ng/ml (23 nmol/L), while age-matched controls averaged
23.3 ng/mL (58 nmol/L). The average 25(OH)D level of the children who developed coronary artery abnormalities was just
4.9ng/ml (12.3 nmol/L).
While acute infections can somewhat deplete 25-hydroxyvitamin D,
through disturbing its creation from vitamin D3 in the liver and due to
more of it being used by the immune system (there's no evidence of this in Han et al, 2016, below), such changes are small
compared to the striking, on-average, deficiency of 25-hydroxyvitamin D
reported by Stagi et al. It is most persuasive that this
deficiency is proportional to disease severity.
It should be obvious that the etiology of KD, MIS-C, PIMS and PIMS-TS is as follows:
- The patient presumably has no helminth infections, and so is prone to excessive, self-destructive, inflammatory responses.
- Since these conditions do not affect most children, or most
children with low 25-hydroxyvitamin D levels, it is reasonable to
assume that those who do contract the condition probably have one or
more relatively unusual genetic factors which make them especially
prone to excessive inflammation.
- The children, as a group, have lower 25-hydroxyvitamin D levels
compared to controls - and the controls usually have levels which are
significantly below the 50 ng/mL (125 nmol/L) required for good immune
function.
- Their low 25-hydroxyvitamin D levels can reasonably be assumed to
drive greater severity of the triggering infection AND more severe
dysregulation of the inflammatory response - see Chauss et al. 2021..
Stagi et al.'s article should have become known to all pediatricians
and immunologists within months. Unfortunately it is in a
paywalled journal, but still this discovery, with obvious, safe, easy
to understand and administer clinical implications should have become
common knowledge for all doctors within a year or two.
However, vitamin D supplementation does not involve the use of any
glamorous, supposedly sophisticated techniques or profitable drugs. So
no one promotes it.
If most children had at least 50 ng/mL (125 nmol/L) 25(OH)D, then it is
obvious that the triggering conditions would either not occur, or would be
tackled more promptly by the children's immune system. It is also
obvious that even with a triggering condition, such children would have
much better regulation of their inflammatory response. So the
vasculitis, artery and organ damage which characterise these
conditions would be far less likely to occur.
Earlier in 2022 I systematically searched for 50 recent articles on
these conditions. One mentioned vitamin D in passing and one
mentioned it as a possibly causative factor. The other 48 did not mention vitamin D. I intend to write to
all the corresponding authors about this. I have never read an
account of these children being treated with vitamin D, or calcifediol
(25-hydroxyvitamin D). They are treated with anti-inflammatory
steroids (which also attenuates innate and adaptive immune responses
to bacterial and viral pathogens) and with specialised transfusions:
intravenous immunoglobulins [
WP] Many of these children suffer lasting heart problems and some die.
This is a travesty. All these conditions are easy to understand, prevent and treat.
We can't give
the children helminths. It is not good enough to give them a few
thousand IU of vitamin D, which takes days to be converted in the liver
to 25(OH)D. Bolus vitamin D3 (such as 2.5 mg 100,000 IU for
a small child) would be helpful, but the best response is a single oral
dose of 0.014 mg per kg body-weight calcifediol, which
is 25-hydroxyvitamin D, and which goes
into circulation in 4 hours, raising levels safely over 50
ng/mL (125 nmol/L) and so enabling the immune system to work properly, or at least to work
much better than with 1/5 to 1/10th of this, as were the
averages reported by Stagi et al.
Treatment for acute disease is beyond the scope of this Call for
Evidence. However, the above discussion shows how out-of-touch
many doctors are about the importance of good 25-hydroxyvitamin D for
the immune system.
Proper vitamin D3 supplementation, for all people (except babies
substantially breast fed by vitamin D replete mothers), from birth,
will entirely, or almost entirely, prevent these and numerous other diseases.
4.6 25-hydroxyvitamin D repletion in acute disease
Doctors and researchers are often
puzzled that attempts to cure acute diseases, including sepsis (which
is not a disease as such, but the body's inflammatory responses being
so wildly dysregulated as to damage multiple organs) with "vitamin D"
do not always produce the desired results.
The reasons for this include:
- By the time treatment commences, a great deal of damage has been
done. So perhaps even a complete restoration of immune system
competency (or its decisive establishment, for the first
time in the person's life) would not be enough to protect the patient
from harm or death.
- Many of these trials use far too little vitamin D3 cholecalciferol.
- Even
those which use the best possible amount of vitamin D
cholecalciferol, such as a bolus dose of 10mg 400,000 IU for 70 kg
body-weight, are not as effective as they ideally would be because the
liver (which may be in a severely impaired state) still takes (very
approximately) 4 days to convert this into the 25-hydroxyvitamin D the
immune system needs. (The kidneys need it too, but they usually
maintain their hormonal 1,25-dihydroxyvitamin D output with 20
ng/mL (50 nmol/L) 25(OH)D.)
- Very few vitamin D intervention trials for acute diseases use the best possible treatment, which is a single oral dose of (very approximately) 0.014 mg calcifediol per kg body-weight.
This boosts 25-hydroxyvitamin D levels safely over 50 ng/mL (125 nmol/L)
in four hours or less, without any reliance on the liver. For
more information see the Front Line COVID-19 Critical Care Alliance's MATH+ hospital protocol: covid19criticalcare.com/covid-19-protocols/math-plus-protocol/ and nutritionmatters.substack.com/p/calcifediol-to-boost-25-hydroxyvitamin, Castillo et al. 2020, described below and #4.7.
Disease treatment is outside the scope of this Call for Evidence, but
it is important to note that many doctors' dim view of vitamin D's role
in preventing or treating disease is due to intervention trials which
do not rapidly replete 25(OH)D levels and due to their own lack of
understanding of how the immune system relies on good 25(OH)D levels.
Rapid 25(OH)D repletion can bring much superior benefits to
conventional steroid-based anti-inflammatory treatments, with few, if
any, risks, with low costs and without the numerous problems (psychosis,
glucose level excursions driving diabetes, etc.) of conventional
treatments.
Two highly successful vitamin D based intervention trials (both RCTs)
involving vitamin D are as follows. These demonstrate the key
role that
rapid repletion of
25(OH)D to ca. 50 ng/mL (125 nmol/L) plays in tacking medical emergencies
which are driven by dysregulated inflammation.
The relative scarcity of such interventions results in and/or indicates at least two things:
- Most doctors do not know that these treatments exist, and are
safe, effective, inexpensive and easy to implement.
(Multinational pharmaceutical companies have no interest in such
research, and benefit from the perception that vitamin D3 and/or
calcifediol are ineffective and/or unsafe.)
- The preponderance of RCTs involving low vitamin D intakes and
their general lack of decisive success leads to the widespread
perception that vitamin D treatment is ineffective in general, or at
least in medical emergencies. This is due to lack of knowledge
about the liver's slow conversion process and the amount of 25(OH)D
which must be generated or otherwise introduced to boost serum 25(OH)D
to proper levels, ideally in hours, rather than weeks or months.
One RCT which deserves to be much better known is:
High dose vitamin D administration in
ventilated intensive care unit patients: A pilot double blind
randomized controlled trial
Jenny E.
Han,
Jennifer L. Jones, Vin Tangpricha, Mona A. Brown, Li Hao, Gautam
Hebbar, Moon Jeong Lee, Shuling Liu, Lou Ann S. Brown, Thomas R.
Ziegler and Greg S. Martin
Journal of Clinical & Translational Endocrinology 2016-04-29
www.sciencedirect.com/science/article/pii/S2214623716300084
There is a
high prevalence of vitamin D deficiency in the critically ill patient
population. Several intensive care unit studies have demonstrated an
association between vitamin D deficiency - commonly defined as serum 25(OH)D below 20 ng/mL (50 nmol/L) - and increased
hospital length of stay, readmission rate, sepsis and mortality.
These patients were all severely ill. They were admitted to ICU,
expected to require mechanical ventilation for at least 3 days and to
remain in intensive care for at least 4 days. 14 were African
American, 15 Caucasian and 1 American Indian / Alaskan. Average
age was about 62 years.
Patients were administered either placebo, 1.25 mg (50,000 IU) vitamin D3 or 2.5 mg (100,000 IU)
vitamin D3 daily for 5
consecutive days. There was
a
significant decrease in the average hospital
length of stay in the two treatment groups compared to the placebo group:
n
|
Total vitamin D3 over 5 days
|
25(OH)D
Day 0
ng/mL
nmol/L
| 25(OH)D
Day 7
|
25(OH)D
Day 14
|
10
|
Placebo
|
21.5
54
| 21.0
53
|
21.3
53
|
9
|
6.25 mg = 250,000 IU
|
23.2
58
| 45.6
114
|
50.5
126
|
11
|
12.5 mg = 500,000 IU |
20.0
50
| 55.4
139
|
63.6
159
|
n
|
Total vitamin D3 over 5 days
|
Average length of hospital stay
(standard deviation)
|
10
|
Placebo
|
36 (19)
days |
9
|
6.25 mg = 250,000 IU
|
25 (14) days
|
11
|
12.5 mg = 500,000 IU |
18 (11)
days |
Bolus vitamin D resulted in a dramatic reduction of days in hospital,
with statistical significance p = 0.03 (time, log transformed).
There is no need to spread the vitamin D over 5 days. Better
outcomes would surely have resulted if it was all taken on day 0.
This is a simple, safe and inexpensive intervention. It should be
very widely used, except for the fact that it takes the liver (very
approximately) 4 days to convert the D3 into circulating 25(OH)D,
assuming the liver is functioning properly, which is not at all
assured. A superior treatment is a single oral dose of
calcifediol, as described next.
It would have been better to boost the patients' 25(OH)D levels earlier in their
illness. It would have been better still if they had healthy, 50
ng/mL (125 nmol/L) or more 25(OH)D levels all their lives. Then
they would have been much less likely to fall ill or (in the case of
injuries which trigger sepsis, such as extensive burns) require hospital care for sepsis at all.
#castillo
A more recent RCT involving
calcifediol
(which
is 25-hydroxyvitamin D) with hospitalised COVID-19
patients, in Cordoba, Spain, is well known to vitamin D aware
researchers and doctors. It should be known by doctors in general
and especially those who treat sepsis, COVID-19, ARDS etc:
Effect
of Calcifediol Treatment and best Available Therapy versus best
Available Therapy on Intensive Care Unit Admission and Mortality Among
Patients Hospitalized for COVID-19: A Pilot Randomized Clinical study
Marta
Entrenas
Castillo, Luis Manuel Entrenas Costa, José Manuel Vaquero
Barrios, Juan Francisco Alcalá Díaz, José López Miranda, Roger
Bouillon, José Manuel Quesada Gomez.
Journal of Steroid
Biochemistry and Molecular Biology (Prepress accepted 2020-08-29)
www.sciencedirect.com/science/article/pii/S0960076020302764
Around April to June 2020, 76 patients admitted to the hospital with confirmed COVID-19 were randomly split into two groups:
26 patients in the control group received no 25(OH)D calcifediol.
50 patients in the vitamin D supplementation group received an oral dose or 0.532 mg 25(OH)D calcifediol (two capsules) on the day of admission, 0.266 mg
on days 3 and 7, and then 0.266 mg every week until
discharge.
In the long term, oral 25(OH)D calcifediol is very approximately
as effective at raising serum 25(OH)D levels as 4 times the mass of
vitamin D3. There is no widely accepted conversion ratio
by which to estimate the equivalent vitamin D3 amount in IUs for a
given quantity of calcifediol. However, if
a factor of 4 is assumed, then this initial oral dose is roughly
equivalent to 2.13 mg vitamin D3, which is 85,120 IU. This
amount, as IUs of vitamin D3, hardly rates as a bolus dose. (I
take
50,000 IU vitamin D3 a week - 69 kg BW.)
The unique benefit of calcifediol over D3 is that it goes straight into
circulation, in 4 hours, as shown in the graph in this patent (page 30 of the PDF), for the
same capsules and dose as used in Castillo et al.
patents.google.com/patent/WO2016124724A1/
.
(2022-06-05 update: This graph was not in the submission Word/PDF files sent before deadline.)
The top graph is from:
Daily oral dosing of vitamin D3 using
5000 TO 50,000 international units a day in long-term
hospitalized patients: Insights from a seven year experience
Patrick J McCullough, Douglas S Lehrer and Jeffrey Amend.
Journal of Steroid Biochemistry and Molecular Biology 2019-01-04
www.sciencedirect.com/science/article/abs/pii/S0960076018306228
(Paywalled.)
sci-hub.se/10.1016/j.jsbmb.2018.12.010
With oral calcifediol, there is no multi-day delay in the liver or reliance on the
liver functioning well. In this trial, there were no
measurements of baseline or later elevated 25(OH)D levels.
However the authors observe that in winter, the average 25(OH)D level
of adults in the Cordoba region is 16 ng/mL (40 nmol/L). (Cordoba
is 37° from the equator, far closer than the UK.)
The patent graph shows mean levels in healthy subjects rising from 18 ng/mL (45 nmol/L) to 62 ng/mL (155 nmol/L) in
4 hours,
going above this somewhat, and back to this after 12 hours, then
declining slowly to 48 ng/mL (120 nmol/L) after 3 days. In this RCT,
the subsequent oral doses would have boosted levels significantly on
and after days 3, 7, 14 etc.
All patients received hydroxychloroquine and
azithromycin. Here are the results:
|
Patients
|
Did not need intensive care
Number Percentage
|
ICU
|
Died in ICU
|
Control
|
26
|
13 50%
|
13 50% |
2
8% |
Vitamin D
|
50
|
49 98% |
1 2% |
None
|
The randomisation resulted in a greater proportion of hypertensive and
diabetic patients in the control group, but the authors state that
their analysis shows that the protective effects of the calcifediol
supplementation remained significant. Age, sex and other
comorbidities were in general much the same in the two groups.
The
validity of these very positive results is supported by a separate analysis by two computational biologist PhDs from MIT.
This rapid-acting oral dose of calcifediol boosted 25(OH)D levels about
as much as the 500,000 IU bolus D3 doses, over 5 days, in Han et
al. 2016. Some part of the dramatic results was due to imperfect
randomisation, but the majority was due to the attainment of the 25(OH)D levels the immune system needs in hours, rather than
days.
Please remember that most "vitamin D" trials involving acute illnesses
involve lower bolus doses of vitamin D3 than Han et. al 2016.
None of these D3 interventions are likely to be as effective as a
single oral dose of calcifediol as described next.
Both these interventions could easily have used twice the amount of D3
or calcifediol. Toxicity from single doses would probably only begin to be a problem with
ten to twenty times these amounts.
4.7 Clinical emergencies: Boosting
25-hydroxyvitamin D safely over 50 ng/mL in 4 hours with a single oral
dose of calcifediol
Further to the above section on Castillo et al. 2020:
The Front Line COVID-19 Critical Care Alliance's MATH+ hospital protocol:
covid19criticalcare.com/covid-19-protocols/math-plus-protocol/
now recommends (following advice of New Jersey Professor of Medicine,
Sunil Wimalawansa) a single oral dose of
0.014 mg calcifediol per kg
body-weight, which for 70 kg is 1 mg. The initially boosted
25(OH)D levels are to be maintained by subsequent vitamin D3 doses in
the following days. There are no RCTs using this protocol.
However, it will surely be more effective than the Han et al. or
Castillo et al. interventions, with no risk of toxicity.
There is no need to test 25(OH)D levels before this calcifediol
dose. The earlier it is used, the better. Please see:
nutritionmatters.substack.com/p/calcifediol-to-boost-25-hydroxyvitamin ,
vitamindstopscovid.info/04-calcifediol/ and Prof. Wimalawansa's article:
#sjw-article .
The success of Castillo et al. is the best current measure (after
discounting for some of the benefit being due to imperfect
randomisation) of the importance of
rapidly, within
hours,
restoring immune system competency by boosting 25(OH)D over 50 ng/mL
(125 nmol/L). The benefits of this rapid repletion is the true
measure of the importance of good vitamin D levels in illness.
It would be better still if no such interventions were needed, due to
all people maintaining such healthy levels through proper vitamin D3
supplementation - meaning that the incidence of such illness will be
very much reduced.
4.8 Vitamin D to suppress inflammatory autoimmune diseases
Further to the above discussion of lack
of helminths driving excessive inflammation, with low 25(OH)D
exacerbating the dysregulated hyper-inflammatory responses, some of the
research articles cited at:
concern the Coimbra, McCullough and Batcheller protocols for treating
autoimmune disorders with more vitamin D3 than is required to attain
healthy 50 ng/mL (125 nmol/L) 25(OH)D levels. The protocols
include other nutrients, low calcium intake, (in some cases) dietary
restrictions and a requirement to drink plenty of water. They are
effective against inflammatory autoimmune diseases including:
- Multiple sclerosis. Amon et al. 2022 report mean
vitamin D3 intakes of 1.32 mg 52,955 IU a day, and 0.742 mg 29,683 IU
for the next 6 disorders:
- Rheumatoid arthritis.
- Psoriatic arthritis.
- Connective tissue diseases.
- Plaque psoriasis.
- Inflammatory bowel
diseases.
- Autoimmune inflammation of the thyroid gland.
- Cluster headaches.
- Migraine.
Such treatment is outside the scope of this Call for Evidence, but we
mention it because it is evident that most people's very low 25(OH)D
levels surely contribute to the incidence of autoimmune inflammatory
disorders in a highly significant way, and that substantial general
relief from these could be expected, without the need for medical
intervention or supervision, if most people supplemented vitamin
D3 properly to attain, in general 25(OH)D levels at or above 50 ng/mL (125 nmol/L).
The list of chronic degenerative diseases in which inflammation plays a
crucial role is long and sobering, not least with Alzheimer's disease
and other neurodegenerative diseases such as Parkinson's disease and
dementia with Lewy bodies.
4.9 Type 2 diabetes, hypertension, breast cancer and cardiovascular disease
This whole section could easily be a dozen times longer.
Please take a look at
vitamindwiki.com.
If even a small fraction of what you read there is true, this is more
than enough evidence that the UK government should revise its guidance
to encourage and support all people to supplement vitamin D3
sufficiently to attain, in general, at least 50 ng/mL (125 nmol/L)
25-hydroxyvitamin D.
Here are four more research items. The
text in violet is direct from this Letter, with inline references to the cited research studies.
The emerging evidence for non-skeletal health benefits of vitamin D supplementation in adults
William B.
Grant, Barbara J. Boucher, Pawel Pludowski and Sunil J. Wimalawansa
Letter to Nature Reviews Endocrinology 2022-02-22
www.nature.com/articles/s41574-022-00646-x
Bill Grant PhD (San Francisco,
CV,
GS) and Professor of Medicine Sunil Wimalawansa MD (
CV,
GS) have been researching vitamin D since the 1990s. Barbara Boucher MD of London (
CV) has been researching vitamin D since 1970:
endocrinologyblog.org/2019/10/18/meet-...dr-barbara-boucher/
Randomized clinical trials
(RCTs) of vitamin D supplementation were mostly designed to test vitamin
D dosage. Heaney’s guidelines for clinical studies of nutrient effects
showed that vitamin D supplementation trials should instead be designed
and analysed by serum concentrations of 25(OH)D. Data from the D2d study
of vitamin D supplementation (4,000 IU per day) in patients with
prediabetes were re-analyzed by achieved serum concentrations of 25(OH)D.
Intratrial
Exposure to Vitamin D and New-Onset Diabetes Among Adults With
Prediabetes: A Secondary Analysis From the Vitamin D and Type 2
Diabetes (D2d) Study
Bess
Dawson-Hughes et al.
Diabetes Care 2020-09-16
diabetesjournals.org/care/article/43/12/2916/30885/
This re-analysis changed negative overall findings for progression to T2DM after vitamin D supplementation
to a hazard ratio (HR) for Type 2 Diabetes of 0.48 (95% CI, 0.29–0.80) for those
who maintained 25(OH)D of 40 to 50 ng/mL (100 to 125 nmol/L) and 0.29 (95% CI, 0.17–0.50) for
those who maintained 25(OH)D > 50 ng/mL (> 125 nmol/L), compared with 25(OH)D levels of 20 to 30 ng/mL (50 to 75 nmol/L) .
One
Canadian observational study involving 8,155 participants investigated
the association between achieved serum concentrations of 25(OH)D and blood
pressure
Evaluation
of vitamin D3 intakes up to 15,000 international units/day and serum
25-hydroxyvitamin D concentrations up to 300 nmol/L on calcium
metabolism in a community setting
S. M. Kimball, N. Mirhosseini and M. F. Holick
Dermato-Endocrinology 2017-04-17
www.tandfonline.com/doi/full/10.1080/19381980.2017.1300213
Participants were given vitamin D3
supplements and counseled on how to achieve 25(OH)D levels > 40 ng/mL (> 100
nmol/L) . Mean baseline 25(OH)D level was 35 ng/mL (87 nmol/L), final 25(OH)D was 45 ng/mL (113 nmol/L) and 33% of participants took > 8,000 IU of vitamin D3
per day. After 1 year, 71% of the 592 participants with hypertension
were normotensive, with 13 ± 19 mm Hg and 11 ± 10 mm Hg systolic and
diastolic blood pressures, respectively, lower than baseline blood
pressures.
Breast
cancer incidence was inversely and significantly correlated with serum
concentrations of 25(OH)D in a meta-analysis using data from two vitamin D
supplementation RCTs and one cohort study.
Breast
cancer risk markedly lower with serum 25-hydroxyvitamin D
concentrations ≥60 vs <20 ng/ml (150 vs 50 nmol/L): Pooled analysis
of two randomized trials and a prospective cohort
Sharon L. McDonnell,
Carole A. Baggerly, Christine B. French, Leo L. Baggerly, Cedric F.
Garland, Edward D. Gorham, Bruce W. Hollis, Donald L. Trump and Joan M.
Lappe
PLoS One 2018-06-15
journals.plos.org/plosone/article?id=10.1371/journal.pone.0199265
The pooled cohort included 5,038 women, 77 of whom were diagnosed with
breast cancer during the studies. Multivariate Cox regression showed
that women with 25(OH)D levels ≥ 60 ng/mL (≥ 150 nmol/L) had a HR for breast cancer of
0.20 (95% CI, 0.05–0.82) compared with women with 25(OH)D levels of ≤ 20
nmol/L (≤ 50
nmol/L).
For
myocardial infarction and all-cause mortality, a 20-year retrospective
analysis of patients of the US Veterans Health Administration with a
baseline 25(OH)D levels of < 20 ng/mL (< 50 nmol/L) with or without counseling to
supplement with vitamin D
The Effects of Vitamin D Supplementation and 25-Hydroxyvitamin D Levels on the Risk of Myocardial Infarction and Mortality
Prakash Acharya, Tarun Dalia, Sagar Ranka,
Prince Sethi, Olurinde A Oni, Maya S Safarova, Deepak Parashara, Kamal
Gupta and Rajat S Barua
Journal of the Endocrine Society 2021-07-15
academic.oup.com/jes/article/5/10/bvab124/6321994
showed that those with a serum concentration of 25(OH)D > 30 ng/mL (75 nmol/L) had
a propensity-matched HR for myocardial infarction of 0.73 (95% CI,
0.55–0.96) and a HR for all-cause mortality of 0.61 (95% CI, 0.56–0.67),
compared with those with 25(OH)D levels < 20 ng/mL (50 nmol/L).
#05-history
5 The UK government's current vitamin D recommendations are based
on the erroneous 2011 US/Canadian Institute of Medicine report
In 2011 the Canadian and US Institute of Medicine published a massive
662 page report, which has been the foundation for most governments'
vitamin D recommendations ever since.
Dietary Reference Intakes for Calcium and Vitamin D
Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium
Editors: A Catharine Ross, Christine L Taylor, Ann L Yaktine, and Heather B Del Valle.
National Academies Press 2011
www.ncbi.nlm.nih.gov/books/NBK56070/
The IOM report contains two enormous blunders:
- The 25-hydroxyvitamin D reference level for vitamin D repletion is set far too low - at 20 ng/mL (50 nmol/L).
- The Recommended Daily Allowance for vitamin D for adults is set far too low, even for this low 25(OH)D reference level, at 0.015 mg 600 IU.
These egregious, harmful, deadly, blunders have never been corrected.
Governments - or rather governments' advisory committees - choose all
the evidence on which they base their final guidance. There is no
reason for any government to follow any document or external
authority. They tend to do so, to anchor their advice to what
they argue, and may believe, is the best available advice of global
experts. However, nothing compels any government to follow the
IOM's or any other body's advice.
Due to the poor quality of the IOM's work, which is at odds with the
recommendation of leading vitamin D researchers - many or most of them
medical doctors themselves, and sometimes professors of medicine -
governments, especially those such as the UK's government, which is
well resourced and has direct access to some of the world's leading
vitamin D researchers in the UK itself, should have developed their own
guidance based on the best available research.
The UK government's failure, so far, to do this has cost UK citizens
dearly - financially and through general ill-health, suffering, lasting
harm and death.
For anyone with moderate expertise and no biases or corrupt interests,
it is not hard to understand the immune system's need for 50
ng/mL (125 nmol/L) 25-hydroxyvitamin D, or to realise that vitamin D3 supplemental
intakes should be specified as ratios of body-weight to reliably attain
these levels in most of the population, without the need for 25(OH)D
testing or other forms of medical monitoring.
All the information required to understand this is public, and is cited
here. If an electronic technician and computer programmer can put
it all together, so should have the various advisory committees,
staffed as they are by professional, highly-qualified, researchers
and/or clinicians, who are both being paid to do this work and in whom
the public places enormous trust.
Leading vitamin D researchers lobbied the IOM to adopt a higher
threshold of 25(OH)D repletion, including for the purpose of ensuring
good immune system health. However, the IOM refused, and made its
recommendations based only on the 20 ng/mL (50 nmol/L) level which it
argued is sufficient to supply the kidneys for the purpose of
calcium-phosphate-bone and skeletal muscle health.
Below are some of the developments before and after the IOM's report in
which researchers argued for a reference level of 50 ng/mL (125 nmol/L )
or thereabouts.
A
Recommended Daily Allowance
(RDA) is a quantity of some nutrient which, if consumed by an entire
population of adults, ensures that 97.5% of those adults will be
sufficient in that nutrient.
This figure is chosen since it means that in the population-wide
distribution curve, all those except the people who fall 2 standard
deviations below the mean, in whatever measure there is of actual
repletion, are the only ones who will not gain sufficient nutritive
value from their daily intake.
There is a lot of scatter in individual responses to nutrients and this
is especially so with vitamin D3 and the resulting long-term 25(OH)D
levels which result from any given vitamin D3 intake for multiple
individuals.
The first reason for this is variations in adult body-weight.
This is highly problematic, since mean body-weights vary between races
and between the sexes:
The mean body-weight of Bangladeshi women is 49.8 kg. Tongan men average 99.4 kg.
In addition, obesity, with its excess adipocytes, including those in
locations where body fat is not normally deposited, presents an
additional difficulty in raising 25(OH)D levels, because this excess
fatty tissue absorbs 25(OH)D from the blood serum, and returns little
of it back if serum levels drop.
There are also individual variations due to genetic and other factors
which affect absorption, hydroxylation in the liver, the degree to
which 25(OH)D is used or broken down by self-limiting mechanisms etc.
The whole idea of an RDA is fundamentally flawed, at least for vitamin
D3, since if it is to work in a given population, the value is set by
the 2.5% of people whose 25(OH)D level rises the least for any given
daily vitamin D3 intake. No regard is taken, at all, of the
outcome for the rest of the 97.5% of the population, except that it is
known to be above the specified threshold of sufficiency.
In order to calculate an RDA, it is necessary to sample a
representative subset of the population (each country's population
differs from that of the next) to survey a range of vitamin D3
intakes, which have been stable for 6 months or more, and then to
measure their 25(OH)D levels. This is difficult enough,
considering some errors in measuring 25(OH)D levels, plus uncertainties
about actual vitamin D3 intakes from food and supplements and the
amount of D3 produced by UV-B skin exposure, which varies seasonally
and in different ways for different people.
Assuming there is such a body of data, which necessarily will involve
thousands of subjects, it is then a straightforward statistical matter
to develop a distribution curve of how vitamin D3 intakes relate to
25(OH)D. The RDA can be calculated by analysing this curve, or a
mathematical representation of it.
The IOM had data from several studies, in order to perform this
analysis. The analysis works from each individual subject's
vitamin D intake and 25(OH)D outcome. This means analysing the
variance of vitamin D3 intakes and 25(OH)D levels,
of each individual subject in all the studies, as a pooled dataset.
However, the IOM took the averages of these measures, of the subjects in each study, and then performed the analysis on the
variance of these averages of the several studies.
In a statistics class, this would result in a big FAIL.
However, no-one noticed the IOM's blunder for several years. By then,
governments all over the world adopted not just the far-too-low 25(OH)D
standard of repletion, but the disastrously low RDA, as mistakenly
calculated by the IOM:
0.015 mg 600 IU.
Two peer-reviewed articles in the highly respected journal
Nutrients exposed the error, with the second group of researchers performing the analysis properly, using their own data.
A Statistical Error in the Estimation of the Recommended Dietary Allowance for Vitamin D
Paul J.
Veugelers and John Paul Ekwaru
Nutrients 2014-10-20
www.mdpi.com/2072-6643/6/10/4472
Letter to
Veugelers, P.J. and Ekwaru, J.P., A Statistical Error in the Estimation
of the Recommended Dietary Allowance for Vitamin D
Robert
Heaney, Cedric Garland, Carole Baggerly, Christine French and Edward Gorham
Nutrients 2015-03-10
www.mdpi.com/2072-6643/7/3/1688
Robert Heaney, who was born in 1927, died in 2016 after six decades of research into osteoporosis and other illnesses:
asbmr.onlinelibrary.wiley.com/doi/full/10.1002/jbmr.2981
They calculated that the RDA (for their particular experimental
subjects) to ensure 97.5% of the people attained at least the (very
low) 25(OH)D level of 20 ng/mL (50 nmol/L), was around:
0.175 mg 7000 IU
Here is an annotated version of Heaney et al.'s Figure 1:
This depicts:
- The IOM's faulty 600 IU RDA (for 20 ng/mL).
- Heaney et al.'s 3875 IU value, also calculated for 20
ng/mL. To arrive at their estimated RDA, it is necessary to add
an additional 3125 IU to account for the sun exposure and vitamin D3
consumed in food by their subjects.
- My estimated intercept for 40 ng/mL (100 nmol/L), at 9110 IU.
Adding the 3125 IU correction to this results in an estimated RDA, for
40 ng/mL, of 0.306 mg 12,235 IU.
Despite the excellent work of Heaney et al. 2015, the veracity of which is not in dispute,
the
IOM has never been corrected and I am not aware of any government
altering its IOM-based advice to account for the very low RDA they
estimated in their egregiously faulty statistical analysis.
We can see from this that any attempt to ensure that 97.5% of a
population of people have at least some healthy level of 25(OH)D,
without any regard to their body weight or obesity status, leads to
unnecessarily high intakes which for people with small bodies and no
obesity, may be excessive.
#50ngml
Here is an account of knowledgeable researchers calling for a 25(OH)D
standard of vitamin D repletion of ca. 50 ng/mL (125 nmol/L):
Cannell et al. 2006 proposed that
50 ng/mL (125 nmol/L) be the target 25-hydroxyvitamin D level, all year round:
Epidemic influenza and vitamin
D
J. J.
Cannell, R. Vieth, J. C. Umhau, M. F. Holick, W. B. Grant,
S, Madronich, C. F. Garland and E Giovannucci
Epidemiology & Infection
2006-09-07
www.cambridge.org/...
The target range of
40 to 60 ng/mL (100 to 150 nmol/L) was stated in
2008 by 48 leading researchers and MDs in the Call to D*Action:
This approximately
50 ng/mL level was fully justified by the research of Quraishi et al.
2014, mentioned at the start of this submission.
This 2020 review article, co-authored by the world's leading vitamin D researcher - Prof. Michael Holick - also calls for
40 to 60 ng/mL 25-hydroxyvitamin D:
Immunologic Effects of Vitamin D on Human Health and Disease
Nipith
Charoenngam, Michael F. Holick 2020-07-15
Nutrients
2020, 12(7), 2097
doi.org/10.3390/nu12072097
40 to 60 ng/mL (100 to 150 nmol/L) was also suggested as the proper target range in this 2019 article (68
citations):
This article also discusses the benefits some people find from much
higher 25(OH)D levels, for suppressing inflammatory disorders such as
psoriasis and rheumatoid arthritis. Please see
vitamindstopscovid.info/06-adv/ for more on this and how it relates to our lack of helminths (intestinal worms).
Here is another recent research article:
Editorial – Vitamin D status: a key modulator of innate immunity and natural defense from acute viral respiratory infections
A. Fabbri, M. Infante, C. Ricordi
Eur Rev Med Pharmacol Sci 2020; 24 (7): 4048-4052 2020-04-05
www.europeanreview.org/article/20876
|
They mention that
40 to 60 ng/mL circulating 25OHD is
required for the autocrine signaling system of immune cells to function properly. The proper term for this is
intracrine signaling. See
vitamindstopscovid.info/02-intracrine/#03-minlev for further discussion of this article.
16 years after the excellent work of Cannell and his highly experienced
colleagues, we still have the UK and many other governments telling
their people, and their doctors, that 20 ng/mL (50 nmol/L) is sufficient
for good health - and that 0.01 mg 400 IU vitamin D3 a day will provide
them with the vitamin D they need to be healthy.
Likewise, 14 years after the 48 leading vitamin D researchers from
multiple countries stated the same thing in the Grassroots Health Call
for D*Action.
People pay their taxes, trust their governments, trust their doctors
and (except for a few autodidacts) utterly depend on the advice of all
these professionals to ensure their good health. Yet, in general,
governments and most doctors, do the bidding of multinational
pharmaceutical companies rather than assiduously pursue the truth about
vitamin D and other nutrients, which would greatly improve the health
of their populations and patients, in ways which are genuinely safe and
effective, but not so profitable for the big corporations.
#06-ratios
6 Vitamin D3 supplemental intake quantities as a ratio of body-weight
I revised this section on 2023-10-01 to
remove some material which is now only of potential historical
interest. You can see the section before these changes at:
This section provides the background to Prof. Wimalawansa's simplified
(August 2023) recommendations for vitamin D3 daily supplemental intake
quantities as ranges of ratios of body weight, with higher ratios for
those suffering from obesity. These recommendations are presented
above:
#00-how-much.
The steps which led to the current recommendations are as
follows. I have mentioned some FLCCC protocols, all of which
should contain good vitamin D3 recommendations. These are listed
at:
https://covid19criticalcare.com/treatment-protocols/
. However it seems that some of them have not been developed in
consultation with Prof. Wimalawansa, or that some which had have since
had his long-term supplemental intake recommendation removed.
- In November 2020 I devised what, as far as I know, is the first
body weight ratio based set of "recommendations" for vitamin D3
supplemental intake, which accounted for the need for higher ratios in
people suffering from obesity:
vitamindstopscovid.info/01-supp/
vitamindstopscovid.info/01-supp/a-ratios/
This was the work of an electronic technician and computer programmer
to develop what I think would be good recommendations, if they were
made by a suitably qualified medical professional. This was
based, as described in these pages and below, on aiming for at least 50
ng/mL 25(OH)D in the great majority of people, using the Ekwaru et al.
2014 research and the Holick et al. 2011 Endocrine Society article.
I proposed, in IUs per day per kg body weight:
Non-obese: 72 to 144
Obesity: 100 to 200
See: vitamindstopscovid.info/01-supp/#ratios.
- While developing this, I analysed the results produced by the Grassroots Health Vitamin D Calculator www.grassrootshealth.net/project/dcalculator/,
which I understand was developed by Samantha Kimball. According
to archive.org, this page first appeared, with a simpler calculator, in
April 2017. My analysis is: https://vitamindstopscovid.info/01-supp/b-grh/
. I entered 1 to 159 kg body weights and a target of 50 ng/mL
25(OH)D. (In 2023-10-02 the calculator enabled inputs of current
supplement among and current 25(OH)D level, but I recall these were not
options in November 2020.)
I found that the algorithm was to produce lower and upper supplemental quantities using this range of ratios:
54 to 144 IU/day per kg
with the quantities rounded to the nearest 1000 IU, and with a maximum quantity of 10,000 IU.
- In December 2020 I added a note in the above page about Afshar et
al. 2020 who obtained good results with a single range of ratios:
70 to 100 IU/day per kg
except that some of their patients, presumably those suffering from
obesity, attained 25(OH)D levels as low as 40 ng/mL. See my
analysis: aminotheory.com/cv19/#2020-Afshar.
- In late December 2021, in a private email discussion list, I suggested:
Non-obese: 70 to 100
Obesity: 108 to 150
- In January 2022, after consulting with Prof. Wimalawansa, the
FLCCC updated their I-MASK+ early treatment protocol (and later their
MATH+ hospital protocol) to:
BMI < 20 (underweight): 40 to 70
BMI 20 to 29: 70 to 100
BMI 30 to 39: 100 to 150
BMI > 39: 150 to 200
I reported this here at 00-evi and argued #underweight
that there was no evidence for people with underweight body types
needing a lower body weight ratio of vitamin D3 to attain any given
25(OH)D level. I also wrote here #obesity-deficit
and in greater detail at: 5nn.info/temp/250hd-obesity/ about the two mechanisms which are thought to cause people suffering
from obesity to require a higher ratio of body weight quantity of
vitamin D3 to attain a given 25(OH)D level.
By early 2023 the I-MASK+ protocol was retired and this long-term
supplemental vitamin D3 intake recommendation was removed in revisions
to the MATH+ protocol. Likewise, the March 2023 I-CARE Early COVID
Treatment protocol does not contain recommendations for long-term
vitamin D3 supplementation, but both retain the 0.014 mg / kg BW single
oral dose calcifediol protocol #4.7, which Prof. Wimalawansa also
recommended in early 2022.
- Prof. Wimalawansa's July 2022 article #sjw-article recommends:
1 to 18 years: 70
BMI < 20 (underweight): 60 to 80
BMI 20 to 29: 70 to 90
BMI 30 to 39: 90 to 130
BMI > 39: 140 to 180
with notes about using higher ratios for non-obese people
who suffer from several auto-immune conditions. The single ratio
for up to 18 year olds does not account for the fact that some children
and adolescents suffer from obesity.
- In February 2023, the FLCCC's I-PREVENT protocol for COVID-19, flu and RSV contains these same recommendations.
The January
2023 I-CARE RSV and flu treatment protocol, the February 2023 I-CARE
insulin resistance protocol and the February 2023 I-RECOVER Long COVID
protocol do not mention vitamin D.
The February 2023 I-CARE For Kids protocol does not mention Prof
Wimalawansa. It recommends the standard 400 IU/day vitamin D3 for
infants younger than 12 months, and the completely inadequate 600
IU/day for "children/adolescents".
The July 2023 I-RECOVER Post Vaccine protocol recommends 4000 to 5000 IU vitamin D3 a day, with no mention of Prof. Wimalawansa.
- In June 2023, The FLCCC published a monologue on cancer care: covid19criticalcare.com/reviews-and-monographs/cancer-care/
and there have been several updates since then. This contains an
extensive section on vitamin D. There is no recommendation on
body weight ratio supplemental vitamin D3 quantities. The text
and a diagram implies that immune cells use "vitamin D" primarily or
wholly in a hormonal manner: circulating calcitriol binding to VDR
molecules on the surface of the cells. This is not the case at
all. Immune cells use 25-hydroxyvitamin D for intracrine and
paracrine signaling. (I am working on suggestions to improve this
important document.)
- As noted above #00-how-much, in his 2023-08-16 FLCCC webinar, Prof. Wimalawansa presented a simplified version of his July 2022 recommendations:
BMI < 30: 70 to 90 Underweight, normal and overweight.
BMI 30 to 39: 100 to 130 Obesity I and II.
BMI > 39: 140 to 180 Obesity III.
There is no precise way of developing such recommendations. They
could be tested, refined or better developed after massive, long-term,
carefully controlled trials with people of many races, body types and
cultures. However, the results would probably not differ much
from these recommendations - and vitamin D3 supplemental intakes need
not be specified with great precision.
I believe this simplified set of ranges of ratios is very good,
provided they are interpreted in a sensible manner. For instance,
a person whose BMI changes from 29 to 30 doesn't suddenly need a lot
more vitamin D3. Likewise from 39 to 40. These
recommendations are by the only vitamin D3 researcher I know of who has
devoted serious attention to the need for such body weight ratio
vitamin D3 supplemental intake recommendations, with higher ratios for
those suffering from obesity. Prof. Wimalawansa has been working
on vitamin D since the mid-1990s and has decades of research and
clinical experience.
It is obvious that nutrient
intakes should be proportional to body-weight in order to attain any
desired level within the body. However, there has
been a paucity of research into vitamin D3 supplemental intakes specified as a ratio of body-weight.
If it were acceptable to have doctors and other healthcare
professionals fussing over everyone's 25(OH)D levels on a continual
basis, then no such ratio-based guidance would be needed. Each
person would adjust their supplemental quantities until their 25(OH)D
blood tests returned values they or their doctor decided were
acceptable.
However, this does not work for babies - or for almost anyone
else. The cost and inconvenience of blood tests is
excessive, and vastly more expensive than the minimal cost of weekly
(to every 10 days) vitamin D supplement capsules or
tablets. (In 2021, I was reliably informed that hospitals
in the USA routinely charged insurers USD$300 per vitamin D
test.) Even if
vitamin D tests were non-invasive and free, this level of medical
involvement is unwarranted.
Pharma grade vitamin D3 costs about USD$2.50 a gram, ex factory.
A 70 kg adult needs about 4 grams if they live to 88. With
widespread adoption, the cost of splitting this vitamin D3 in to once a
week, or once every 10 days, capsules need not be high. Every 10
days for 88 years is 3214 capsules, which would cost USD$100 or so to
manufacture, and more to package and distribute. Doctors in
developed countries might be happy to run 25-hydroxyvitamin D blood
tests and advise their patients accordingly, but in many countries,
there are almost no doctors, very few nurses - and test labs are 1000
km or more away.
This is nutrition, not medicine. We need simple guidance, applicable to
everyone
on how much vitamin D3 to take, without the need for medical
monitoring, with certainty of attaining at least 40 ng/mL, and ideally
over 50 ng/mL 25(OH)D, without danger of toxicity. These
recommendations are for all people who do not have any health condition
which should, ideally, be medically managed in ways which affect
vitamin D3 supplementation,
The question is how to devise such guidance, which any literate and
minimally numerate person can follow, to ensure that most people
(ideally everyone, but this is impossible - 90 to 95% would be good)
supplement enough vitamin D3 at all stages of their life, to maximise
their health.
There is a wide range of 25(OH)D levels which will ensure this, except
for those with autoimmune inflammatory disorders who generally need
more than 50 ng/mL (125 nmol/L) 25(OH)D to suppress these symptoms, in
the absence of helminths.
vitamindstopscovid.info/06-adv/
The situation is made much easier by the very wide gap between the
minimal level 50 ng/mL (125 nmol/L), as just mentioned, and the level three times this - 150 ng/mL (375
nmol/L) at which toxicity may become a problem for some people.
The situation is made easier still by the strong self-limiting nature
of the activity of the 24-hydroxylase enzymes which degrade 25(OH)D in
proportion to its level.
So despite widespread, ill-informed, fears of toxicity, vitamin D is a
relatively easy nutrient to choose intake quantities for, without any
medical involvement. This can only be done by basing it on ratios
of body-weight, with different ratios for those suffering from obesity.
Ideally there would have been multiple trials of body weight ratio based vitamin D
supplemental intake quantity protocols. ("Supplemental intake" is
appropriate. This is nutrition. "Dose" is appropriate for
medicine.)
As far as I know, only one such research study has been
published. Iranian MDs at a hospital in Dubai, UAE have been
using
ratio-based
vitamin D3 supplemental quantities since 2010 with some opthalmology
patients, and, with great success since early June 2020 with all their
COVID-19 patients.
Suggested role of Vitamin D
supplementation in COVID-19 severity
The authors are directors at Iranian Hospital Dubai, Dubai, UAE:
Parviz
Afshar, Hospital Director, Mohammad Ghaffaripour, ICU
Director and Hamid Sajjadi, Neuro-Ophthalmology Director.
Journal of Contemporary Medical Sciences Vol 6 No 4 (2020):
July-August 2020 2020-08-26
www.jocms.org/index.php/jcms/article/view/822
(3 years later,
cited by only two articles, neither of which concern body weight ratios.)
This short article is packed with interesting items. Highlights include:
- 500+ neuro-opthalmology patients. Unsupplemented, 95% had 25(OH)D levels below 35 ng/mL (87.5 nmol/L).
- Ratio-based vitamin D3 supplemental intake quantities of 70 to 100 IU D3/day per kg body-weight.
- Supplemented on this basis since
2010, all attained at least 40 ng/mL (100 nmol/L) with none over 90 ng/mL (225 nmol/L).
Unsurprisingly, this involved no toxicity. (However, I have been
reliably informed by an Australian MD that she would expect some people
to exceed this upper 25(OH)D level with these intakes.)
- 21 patients (including 2 healthcare workers and several with
chronic disease) who had > 40 ng/mL (100 nmol/L) 25(OH)D and who had COVID-19
reported maximum stays in hospital under 4 days.
- In early June 2020 they started supplementing all COVID-19
inpatients with 7.5mg 300,000 IU intramuscularly plus
(presumably oral) D3 at 100 IU/day/kg == 0.0025mg/day/kg. For
a 70kg person this is 0.175mg 7000 IU/day. This is in addition
to hydroxychloroquine, Remdesivir and other treatments. This
resulted in:
. . . a dramatic and complete
resolution of ICU admissions was observed in the last 8
weeks.
We cannot over-emphasize the role of Vitamin D in
controlling all infectious diseases especially in COVID-19.
We had no patients with initial Vitamin D levels of
> 40ng/mL (100 nmol/L) that required more than 2 to 3 days of
hospitalization, hence no cytokine storm, hypercoagulation,
nor complement deregulation occurred.
Prior to this change, we had several deaths of COVID-19
patients on respirators.
They recommend 70 to 100 IU/day/kg ratio-based D3 supplemental
intake for all people, with a potential simplification for people
between 50kg and 100kg: to a 1.25mg 50,000 IU capsule per week,
which is 0.178mg 7143 IU / day. (143 to 71 IU/day/kg.)
For people with < 30 ng/mL (75 nmol/L) 25(OH)D, they recommend 7.5mg 300,000
IU
D3 intramuscular injection, followed by body-weight ratio-based daily
intakes. However, without the initial injection, such people would
still reach the desired range of 25(OH)D levels after several
months. A bolus D3 starting dose would achieve the same goal of
earlier repletion, which would be especially valuable in an environment
of threatening infectious disease.
For people with 30 to 40 ng/mL (75 to 100 nmol/L) they recommend just
the ratio-based intakes. For people with > 45 ng/mL (112 nmol/L) they suggest
retesting after a few days to check for a possibly erroneous
initial reading, and then testing every 4 months after that. Below, by "normal" they mean "healthy".
. . . we would like to propose changing
the VDL to 40 to 100 ng/mL as normal and consider below 40 ng/mL as
deficient.
Restating this in nanomols per litre:
. . . we would like to propose changing
the VDL to 100 to 250 nmol/L as normal and consider below 100 nmol/L as
deficient.
Sidebar on the journal and Iranian research:
The Journal of Contemporary Medical Sciences (about) was
launched in 2015 and is a quarterly peer-reviewed open access
publication of Nab’a Al-Hayat Foundation for Medical Sciences and
Health Care, Iraq.
I am wary of journals I have never heard about from non-Western
countries, but this is legitimate, being listed
in Index Copernicus and not mentioned in this list of predatory
journals: olddrji.lbp.world/administrator/RejectedJournals.aspx. This not-for-profit hospital is the oldest in Dubai www.ihd.ae/about-us
and is primarily staffed by Iranians. en.wikipedia.org/wiki/Iranian_Hospital,_Dubai
.
This is the latest in a long line of excellent nutrition research
I have read from Iran and/or Iranians
On this basis I believe we can tentatively assume that:
70 to 100 IU D3/day per kg body-weight
as a good range of ratios for a global, all ages, all body weights, vitamin D3 supplemental intake protocol, for people who
do not suffer from obesity, without the need for testing or medical supervision, except as required due to possible or actual ill-health.
Here is some terminology for the range of ratios:
70 IU / day per kg body-weight is the base ratio.
100 IU / day per kg body-weight is the upper ratio.
Devising such a protocol as this and having it adopted by most people,
worldwide, would end what is often referred to as the "vitamin D
deficiency pandemic" and bring enormous health and happiness benefits.
This simple range of ratios can be improved upon by devising a
correction factor to account for the widely and uncontroversially
recognised problem faced by people suffering from obesity: that their
25(OH)D levels are significantly lower than those which would result
from the same vitamin D3 intake as ratios of body-weight for people who
were not suffering from obesity.
The problem seems to be obesity, not being simply overweight.
Definitions of overweight, obesity and morbid obesity are problematic,
since the BMI formula has long been known to overestimate obesity in
tall people, and so underestimate it in short people, including babies,
children and adolescents. In this discussion we have no precise
definition of obesity I, II and III. Waist vs. height and
clinical assessment may be more appropriate than BMI for determining
this. Obesity is a serious over-inflammatory metabolic
disorder which requires medical attention. In such circumstances
doctors may well make specific nutritional decisions.
#ekwaru
The best research article on which to base judgments about an "obesity correction factor" is:
The Importance of Body Weight
for the Dose Response Relationship of Oral Vitamin D
Supplementation and Serum 25-Hydroxyvitamin D in Healthy
Volunteers
John Paul Ekwaru, Jennifer D. Zwicker, Michael F.
Holick, Edward Giovannucci and Paul J. Veugelers.
PLoS One
2014-11-05
journals.plos.org/plosone/article?id=10.1371/journal.pone.0111265
Here is an annotated version of their Figure 3, from the PDF version of
the article, which for some reason does not appear in the HTML
version.
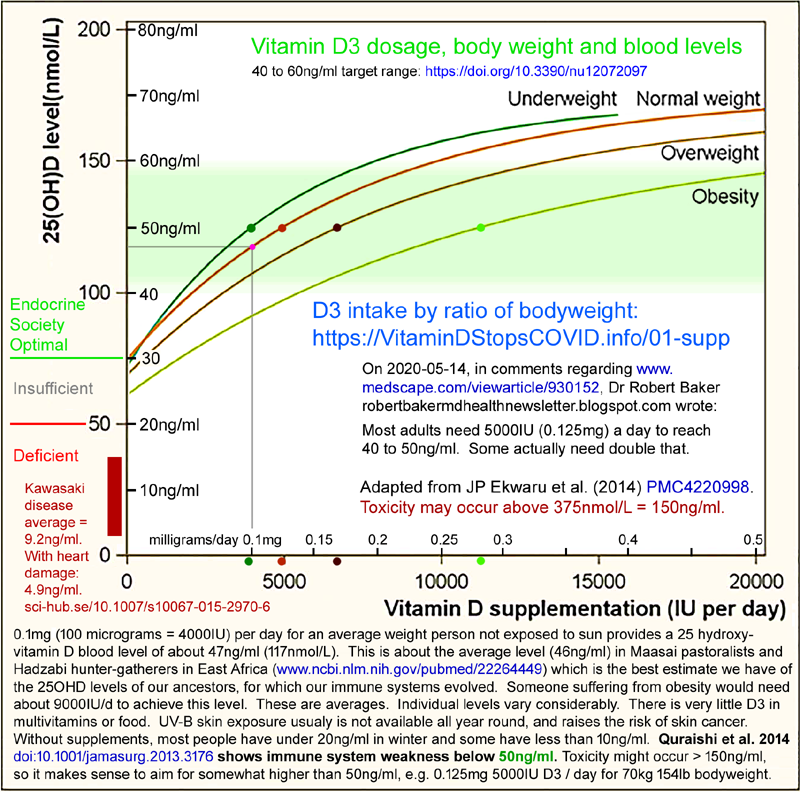
These four curves are averages of 22,214 25(OH)D blood tests from
17,614
healthy North American adults participating in a preventive health
program. So this is a self-selected sample of the
population. "Underweight" "normal weight", "overweight" and
"obesity" are therefore self-described items of data, rather than based
on clinical judgments made in a consistent framework. These
subjects would also have obtained some vitamin D3 from sunlight,
fortified food and multivitamins.
We assume a normal body-weight of 70kg (154lb),
while recognising that normal body-weights (not average - normal,
healthy, non-overweight, non-obese) body-weights for Asians are somewhat
less than this. (
en.wikipedia.org/wiki/Human_body_weight
indicates that Bangladeshis' average body weight is 52.5 kg and that
Tongans' is 98.5 kg. However these populations are far too often
underweight and obese respectively.)
For 70 kg body-weight, 5000 IU / day is close enough to 70 IU/day/kg. We see
from the Ekwaru et al. graph that this results in average 25(OH)D levels of 50 ng/mL (125 nmol/L).
The self-limiting mechanisms which control 24-hydroxylation of 25(OH)D
are evident in all four curves flattening out at higher 25(OH)D
levels. This means that the
upper ratio, 100 IU/day/kg, which is
1.43 times the base ratio, will not result in mean 25(OH)D levels of 1.43
times 50 ng/mL (125 nmol/L). Indeed, the intercept from 7000 IU
with the "Normal weight" curve gives a level of about 58
ng/mL (145 nmol/L). This leveling off of the slope of these curves would be
called "compression" in electronics. It makes our task much
easier than if 25(OH)D levels rose linearly in proportion to vitamin D3
intakes.
Our task now is to determine what, if any, correction factor to apply
to the initial range of ratios (70 to 100) to make them more suitable for people
who are overweight, or suffering from (self-described) obesity, in a
context where there was no separate option to report "morbid obesity", now known as "obesity III".
This requires some judgments about to what extent, at 50 ng/mL (125
nmol/L), the vitamin D3 intakes for the "Overweight" and "Obesity"
curves
indicate that the extra vitamin D3 requirement to attain this level is
out of
proportion to the extra weight, for adults, implied by being
"overweight" or "obese". This is tricky given the lack of formal
definitions and the self-described nature of these data.
#ek-2.5-and-2-to3
Fortunately, Ekwaru et al. have quantified this:
We recommend
vitamin D supplementation be 2
to 3 times higher for obese
subjects and 1.5
times higher for overweight subjects
relative to normal weight subjects.
It is a common error of expression to use "times higher" rather than
"times the (whatever the reference item is)". So we
interpret these statements as meaning:
Overweight people should supplement 1.5
times the amount of vitamin D3 normal weight people need.
People suffering from obesity should supplement 2
to 3 times the amount of vitamin D3 normal weight people need.
They mention "two to three times more" in their abstract,
citing the Endocrine Society
,
and note that their article is intended to provide a research basis to
justify this, which the Endocrine Society acknowledged was lacking. They
are referring to the Endocrine Society's 2011 guidelines, which remain
current in 2023:
Evaluation, Treatment, and Prevention of Vitamin D Deficiency: an Endocrine Society Clinical Practice Guideline
Michael F.
Holick, Neil C.
Binkley, Heike A. Bischoff-Ferrari, Catherine M. Gordon, David A.
Hanley, Robert P. Heaney, M. Hassan Murad and Connie M. Weaver
Journal of Clinical Endocrinology & Metabolism
2011-07-01
academic.oup.com/jcem/article/96/7/1911/2833671
This article recommends the IOM's mistaken 600 IU RDA for all but
those with obesity and those on particular medications. Holick et al.'s terminology
regarding higher intakes for those with obesity involves
similarly awkward and imprecise expression:
(2.5) We suggest that obese children and adults
and children and adults on anticonvulsant medications,
glucocorticoids, antifungals such as ketoconazole, and
medications for AIDS be given at least two to three times
more vitamin D for their age group . . .
[Normal weight] . . . maintenance
therapy of 1500 – 2000 IU/d.
From their page 1924 restatement of rec. 3.5:
3.5 In obese patients, patients
with malabsorption syndromes, and
patients on medications affecting vitamin D metabolism, we suggest a higher dose (two to three
times higher; at
least 6000 –10,000 IU/d) of vitamin D to treat vitamin D deficiency to maintain a 25(OH)D
level above 30 ng/mL, followed by
maintenance therapy of at least 3000
– 6000 IU/d.
They clearly mean "2 times" to "3 times" the:
[Normal weight] . . . maintenance
therapy of 1500 – 2000 IU/d.
Table 3 shows in the right two columns the Endocrine Society
recommendations alongside the sliced and diced arrangement of the
IOM in the middle. For adults 19 years and above, the Endocrine Society daily requirement is
1500 to 2000 IU/d, with 10,000 IU being the Endocrine Society "upper level", with
nothing about obesity, since this is not an element of the Endocrine Society's recommendations.
"Average weight" means a BMI of 18.5 to 20 - so we assume an
average BMI of
19.25.
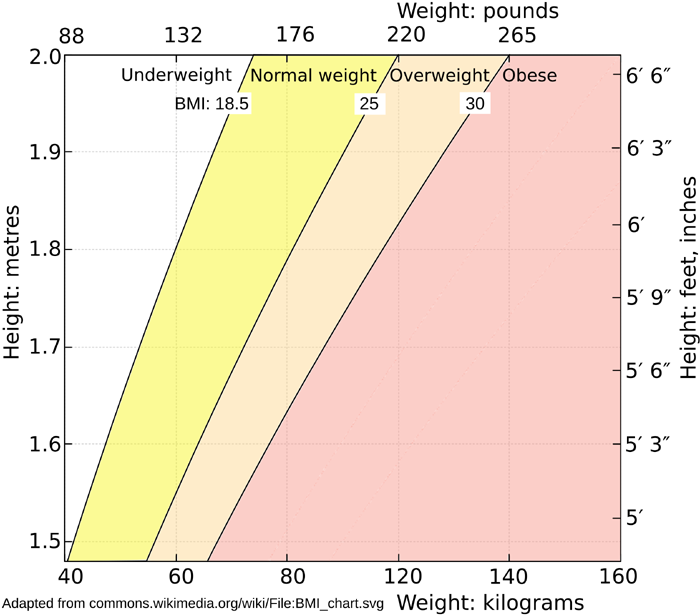
The average BMI of overweight people is 25 to 30 = an average
of 27.5, which is 19.25 x 1.425.
So on this basis, we don't need a ratio different from the
normal weight range of ratios, 70 to 100 IU/day/kg, for overweight people to achieve their goal of 1.5 times the vitamin D3 intake of
average weight (non-overweight) people. (This 1.5 is from our above reinterpretation of the statement by Ekwaru et al. #ek-2.5-and-2-to3.)
Obesity is open ended: BMI > 30. (The above chart has no
category for obesity III, AKA "morbid obesity".) If we take the
mid-point of another step of 5 upwards, this is 32.5 as the low end of
obesity = 19.25 x 1.69.
To match this with a low end target of 2 times the average weight D3
intake (where 2 is from the above re-interpretation of the statement by Ekwaru et al. #ek-2.5-and-2-to3), we need a ratio (2.0 / 1.69) = 1.1834 x the amount of vitamin D3 ordinary weight people take.
If we assume that the average high end of obesity is
another 5 above this: 37.5 = 19.25 *
1.948. Ekwaru et al. suggest (in our reinterpretation,
above, of their statement) that people suffering from obesity need 3 times the average weight D3
intake, so we need a ratio (3.0 / 1.948) = 1.54 x the amount of vitamin D3 ordinary weight people take.
Since there is such a high safety margin, since some people may
benefit from higher intakes and since aiming for 50 ng/mL means
half the people will have less than this, we can adopt approximately 1.50 as the correction factor for obesity, to be applied to the initial Afshar et al. ratios above:
For people suffering from obesity:
70 x 1.43 = 100 IU / day per kg body-weight is the base ratio.
100 x 1.5 = 150 IU / day per kg body-weight is the upper ratio.
This is a somewhat reverse engineered argument to show that Prof.
Wimalawansa's recommendations, and my own suggestion for what
recommendations would be, are very approximately valid.
Since the original data had no option for obesity III (morbid obesity), and since
people suffering from this may not have been well represented in the
dataset, Prof. Wimalawansa chose to make another range of ratios
approximately 2.0 times that of the ratios for normal weight people, to
suit those with the open ended, but clinically perilous, diagnosis of
obesity III.
2022-07-09 update: No evidence for lower ratios for underweight body morphology
#underweight
There is no observational evidence that people with normal body-weight
morphology have a deficit of 25(OH)D in a manner which does not affect, at
least to the same degree, people with underweight body morphology (who
have less adipose tissue).
This can be ascertained from the Ekwaru et
al. 2014 graph above, where the dots representing the quantities of
vitamin D3 required to reach 50 ng/mL 25(OH)D are spaced horizontally
in approximate proportion to the average body-weights of adults who are
underweight, normal weight and overweight, respectively. The same
is
not true of the dot for people who indicated that they suffer from
obesity. That dot is far to the right of where it would be if the
same body-weight ratios of vitamin D3 generally lead to the attainment
of 50
ng/mL 25(OH)D in obese people just as is the case for underweight,
normal weight and overweight body morphologies.
These and prior observations are the basis for Holick et al. 2011's
and Ekwaru et al. 2014's statements about vitamin D3 being needed for
adults suffering from obesity being 2
to 3 times that required for adults with normal body-weight.
2022-07-9 update: Current research on the reasons for people
suffering from obesity to have lower than expected 25(OH)D levels, for
a vitamin D3 intake commensurate with their body weight
#obesity-deficit
The following is an account of the most
recent research. It is not a thorough review of the field, which goes
back well before 2010, when the lower than expected 25(OH)D levels in
obesity were well known. A fuller account of the research is at
this temporary page:
5nn.info/temp/250hd-obesity/. The summary is:
Roizen
2019:
In female mice fed a high-fat diet which made them obese:
Lower levels of 25-hydroxylase enzyme mRNA in the liver.
Likewise, significantly less of this enzyme was found in
the liver.
No such reductions in mRNA for three other enzymes which
are related in some way to 25(OH)D.
With similar levels of circulating vitamin D3
cholecalciferol to the control mice, the obese mice had
about 50% less circulating 25(OH)D.
Homogenized liver samples from the obese mice had only
1/3 the 25-hydroxylasing activity of such samples from
control mice.
They state (I did not chase the references) that this
reduction in the 25-hydroxylase Cyp2R1 gene mRNA
transcription is caused by:
. . . chronic inflammatory process
induced by obesity that involves both innate and acquired
immunity, and which is associated with marked increases in
circulating cytokines.
They do not establish that the changes are due to obesity
itself, rather than partly or wholly the changed diet.
There is no attempt to link this to humans, but I think
that it is reasonable to tentatively assume that similar
processes happen in humans, due to obesity and/or dietary
changes.
Lekhwanky
et al. 2020:
In male and female mice fed a high-fat diet which induces
obesity:
80 to 90% less 25-hydroxylase enzyme mRNA in the liver.
~65% less of this enzyme in the liver.
In four morbidly obese women who kindly consented to
abdominal adipose tissue biopsies before and after Roux en Y
bariatric weigh loss surgery, which successfully reduce
d their obesity:
All four subjects had a 50% increase in 25-hydroxylase
enzyme mRNA in this tissue 11 to 19 months after surgery
relative to pre-operative levels.
The researchers argue that similar changes in mRNA
expression, due to obesity itself (or, I think, perhaps due
to the pre-operative diet and absorption, which differs from
the post-operative), might be found in the liver. They also
argue that tissues other than the liver play a greater role
in production of circulating 25(OH)D than is generally
recognised.
I regard this, in combination with the mouse research, as
good evidence that the 25(OH)D deficit in obesity is
substantially caused by reduced hydroxylation of vitamin D3
to 25(OH)D.
Zhu
et al. 2021:
Mouse experiments confirm the above, but the authors argue
(I have not tried to follow the details) that the reduced
25-hydroxylase levels in the liver are caused by the changed
diet, rather than by the resultant obesity.
I regard these articles as good evidence that the 25(OH)D
deficit is substantially caused by reduced 25-hydroxylation.
Since this is all to do with obesity, or obesity-inducing food,
this has nothing to do with any putative 25(OH)D deficit in
normal weight people in comparison to underweight people with
less ordinary adipose tissue.
For further information on the Coimbra protocol for treating
auto-immune inflammatory disorders such as multiple sclerosis (MS),
Crohn's disease, ulcerative colitis, vitiligo, psoriasis, rheumatoid
arthritis, cluster headaches and migraine, please see the articles
cited at
vitamindstopscovid.info/06-adv/#01-higher - especially
Amon et al. 2022.
As Prof. Wimalawansa notes (page 14 of his July 2022 article) the Coimbra protocol involves
reducing calcium intakes. It also involves regular monitoring of
calcium and parathyroid hormone levels.
Despite most doctors being very concerned about 25-hydroxyvitamin D
levels, Amon et al. do require that their patients have this
tested. The mean vitamin D3 intake of their non-MS patients was
0.75 milligrams 30,000 IU / day and for their MS patients, 1.33 mg
53,000 IU / day.
On 2022-09-18 I don't have any substantial research to cite regarding this, but the generally recommended
calcium
supplemental intakes are intended for people who were not
supplementing with much, or any, vitamin D3. It may be that
less or no calcium supplementation is required with the 50 ng/mL or
more 25-hydroxyvitamin D levels which the above guidance will generally
achieve and that this may be healthier in the long term than the
currently widely accepted calcium supplemental quantities.
#07-fortif
7 Fortifying food with
vitamin D3 can only provide a small fraction of what people need.
Government efforts should be directed entirely at facilitating proper
supplementation.
The following arguments are a mixture
of those against food fortification in general, and those specifically
against fortifying food or drink with vitamin D3.
Perhaps there are some circumstances in which government support for
fortifying food with vitamin D might be justified. We can't think
of any. Please consider all these arguments before proposing that
food or drink be fortified with vitamin D3.
- Fortification alone cannot deliver enough vitamin D3 to attain the 25(OH)D levels required
for proper immune system function. More on the limited quantities below.
- Consuming fortified foods will give many people a false sense of security about their own vitamin D status. This will reduce
the impetus to supplement vitamin D3 properly.
- Governments, doctors, nutritionists and anyone selling food or
drink should not portray the very limited quantities of vitamin D which
can be included in fortified products as providing any significant
health benefit.
While it is true that if a person has extremely low 25(OH)D levels, to
the point of this causing rickets or other forms of bone weakness, the
small quantities of vitamin D3 (or perhaps D2) in fortified food will
probably be helpful. Any improvement on levels below 10 ng/mL (25
nmol/L) will reduce such harm.
However, the larger problem is immune system health. The
quantities of vitamin D3 which are available through fortification are
dwarfed by every person's real needs.
In principle it would be acceptable to fortify foods and label them appropriately, such as:
This product contains 0.002
milligrams (80 IU) of vitamin D3 per 250mL serving. Daily use of
this product may make a clinically significant improvement in cases of
extreme vitamin D deficiency which disrupt bone development and
maintenance. However, this is about 1% of the amount of vitamin
D3 an average weight adult needs to maintain immune system health.
This is not the sort of text anyone wants on a carton or bottle of milk.
- Supplementation is inexpensive - such as with 1.25 mg 50,000 IU
tablets or capsules once a week, for 0.18 mg 7,143 IU per day (70 kg non-obese BW) or more or
less frequently according to body-weight.
eBay's best UK source
is www.ebay.co.uk/itm/163671096717 £30, including postage, for 90 50,000 IU capsules from BIOINNOVATIONS PHARMACAL. Bio-Tech Pharmacal Vitamin D3-50 is
half this price for 100 capsules, but no-one in the UK sells it,
so there is a shipping cost from the USA.
With widespread adoption, prices would fall and a range of capsules or
tablets would be available with minimal markups and no shipping costs
from all supermarkets. 100x 1.25 mg 50,000 IU tablets or capsules
contains 1/8 of a gram of vitamin D3 - and it costs USD$2.50 a gram
ex-factory. In British currency, this is about £0.25 worth of
vitamin D3. The costs of tablets, packaging, testing,
distribution, wholesale and retail markups and tax mean that the total
retail cost per 100 capsules, (enough for two 70 kg people for almost a
year) need not be more than a few pounds. For instance Tesco has
90 folic acid tablets for £1.50. So it can't cost a lot to make small tablets.
The current costs of vitamin D tablets, such as £3.50 for 90 x 1000 IU or £8.00 for 96 x 2000 IU
(EXTRA STRENGTH) are ruinous. 5000 IU a day with the 2000 IU
tablets is 912 a year = 9.5 bottles = £76 a year per person.
Double or triple this for heavier body-weight or those suffering from
obesity, who need a lot more than 5000 IU a day.
- The costs of food fortification cannot be justified, even if this was able to
attain the same 25(OH)D levels in general, which is not the case. Those
costs fall on food and drink producers and so must be borne by
all people who buy these products, including those who are supplementing vitamin D3
properly.
- Vitamin D3 (or the less
effective
D2) is subject to degradation in foods and perhaps drinks in
storage and with cooking.
- Not all food made is consumed, so fortification is inefficient.
- Fortification cannot be applied to organic food, or any fresh
fruit, vegetables, fish, other seafood, poultry or meat. It
is primarily applicable to starchy, oily, foods and cooking oils, which are of limited benefit to
health and may be harmful.
- No food or drink product is used consistently by any particular
sub-division of the population which it might be intended to
help.
Milk is probably the most common product to be vitamin D (D2?)
fortified. While this was important a century ago in reducing the
incidence of rickets, many people do not drink milk. Most East
Asians are unable to digest lactose, so they avoid it unless in
rare cases lactose free milk is available. As we age (RW's
experience in recent decades) we can become lactose intolerant.
According to en.wikipedia.org/wiki/Lactose_intolerance
the term "intolerance" is a medicalisation of a natural pattern
of lactose malabsorption which affects 60 to 70% of the world's adults.
Likewise cooking oils, except perhaps in cultures where their extensive
use is ubiquitous. Likewise butter and other such spreads.
- Even if fortification of multiple foods were actually able to
deliver enough vitamin D3 per day, the use of fortified products is so
varied between multiple individuals that there is no way it could be a
reliable source of vitamin D3 for all people.
- Fortification by government mandate or encouragement is
arguably government overreach.
- Fortification would only be practical for foodstuffs produced in
the country of consumption, unless it was possible and cost-effective
to have producers in other countries make special batches of their
product, fortified to the standards and testing requirements of the
country in which it is to be consumed.
- Similarly, mandating fortification for locally produced
foodstuffs imposes not just the direct cost of fortification on the
manufacturer, but further costs regarding production, warehousing and
distribution if they are also to sell unfortified products to other
countries, or to customers in their own countries if the fortification
regime allows such unfortified products to be sold.
Here is a recent article which argues for vitamin D fortification of milk in Australia:
Vitamin
D Fortification of Milk Would Increase Vitamin D Intakes in the
Australian Population, but a More Comprehensive Strategy Is Required
Eleanor
Dunlop and nine colleagues
Foods 2022-05-09
www.mdpi.com/2304-8158/11/9/1369
The authors work on the basis of 25(OH)D levels below 20
ng/mL (50 nmol/L) being "low" - - the same as used in the
UK - and state that 15% to 32% of the adolescent and adult
population falls below this threshold. Rates of deficiency, by this very low standard, are higher in
winter in the southern states and in remote-dwelling indigenous people
- who mainly live in sunny central and northern parts of the country.
The authors model fortification of "fluid dairy milks and alternatives"
with 0.8 ug 32 IU vitamin D per 100 mL and conclude that this would
increase average vitamin D intake by
2 ug 80 IU per day. (This seems plausible, but only a subset of the population drinks milk or soy etc. alternatives.)
They estimate that current average vitamin D (D3 and, curiously,
25(OH)D) intakes are equivalent to 1.8 to 3.2 ug a day (72 to 128
IU/day) vitamin D3. They assume that the IOM's 10 ug 400 IU / day
vitamin D3 recommendation is adequate.
Even with these far too low standards of vitamin D3 intake and 25(OH)D
levels, they conclude that their proposed fortification arrangement
"would be insufficient to ensure that most of the population
achieves" the IOM recommended intake.
Anyone seriously contemplating vitamin D fortification must not only
consider it in light of the real intake requirements to ensure immune
system health, but should also scrutinise the detailed guidance for
such fortification from the W.H.O. This 376 page book
remains current to this day.
The authors assume that low vitamin D status is indicated by 25(OH)D
levels below 11 ng/mL (27.5 nmol/L), which is less than a quarter of the
real threshold. They mention that vitamin D fortified milk in the
USA since the 1920s has not been so successful with "some elderly
individuals and some black populations" due to their low intakes of
fortified dairy products.
On page 130 - 131:
Either
vitamin D2 (ergocalciferol) or D3 (cholecalciferol) can be added to
foods. The two forms have similar biological activities and both
are very sensitive to oxygen and moisture, and both interact with minerals.
. . . vitamin D fortification of milk and margarine have been found to be useful strategies for increasing intakes; the goal is to supply up to 5 ug 200 IU/day in the total diet.
Pages 135 to 330 cover all the technical, administrative, legal,
quality control, labeling, cost effectiveness, education, marketing,
industry communication and international foods standards considerations
which must be part of any government-mandated food fortification.
We argue that all such effort to enact compulsory food fortification
with vitamin D - or even to permit and monitor it on a voluntary basis
- would be not just a waste of public resources, but produce close to
zero benefit for the public, impose costs on business and so on many
sectors of the public and, most crucially, provide a dangerously false
assurance to the public that they can obtain sufficient vitamin D3 from
food to not need proper supplementation.
Except for infants substantially breast fed by vitamin D replete
mothers and those few individuals who for some reason have high levels
of UV-B skin exposure all year round (which should be discouraged due
to the skin damage and cancer risk) every individual in the UK or in
any other country far from the equator can only assure good immune
system function by supplementing vitamin D3 according to the body-weight
ratio guidelines mentioned above. This supplementation requires
no medical supervision or 25(OH)D testing.
Government effort should be focused entirely on facilitating this supplementation.
Since there seems to be no precedent for community-wide adoption of any
nutritional supplement, it is easy to criticise our proposal for daily
to weekly to thrice a month vitamin D supplementation, for essentially
all people, of all ages, as impossible or at least unlikely to
succeed.
However, through individual choice and the encouragement of governments, norms of social behaviour do change.
Most people now avoid drinking alcohol before driving. Few people
smoke compared to past decades. Almost no-one would feel
comfortable not wearing a seatbelt in a car - yet no-one wore them 60
years ago. These are sensible changes.
En-masse flexibility of public and private behaviour has been
demonstrated recently regarding acceptance of masks, social distancing,
lockdowns and rapidly developed, inadequately tested, COVID-19 vaccines.
Some of these changes in normal behaviour were chosen willingly based on
realistic information. Other changes were forced on the public by
law and by misleading and manipulative information campaigns.
Vitamin D is well known, highly regarded, well researched and tested,
with a very wide margin of effectiveness between the amount which is
required and that which might cause harm. It is not a new
product. It is not a drug. It is not the product of major
pharmaceutical companies. It is extraordinarily inexpensive,
other than the minor cost of forming into tablets, capsules or drops.
Vitamin D deficiency is ubiquitous and causes pervasive
ill-health. This deficiency is much easier to fix than the
deficiency of almost any other nutrient. For instance, zinc
must be taken every day. Determining the correct intake of iron
is difficult without medical advice, since the body has no way of
excreting it if the intake is excessive.
Widespread vitamin D repletion will reduce ill-health very
substantially. Whether the impact will be 20% or 50% cannot be
known, but pervasive productivity and happiness benefits will occur
together with lowered healthcare expenses, regarding treatment and
reduced need for mass vaccination campaigns.
It has always been more effective, and safe, to replete vitamin D than
to give flu vaccines to a large fraction of the population every
year. The same applies to COVID-19.
The UK once lead the world in vitamin D research and the eradication of
the scourge or rickets. But rickets still occurs, flu infections
still harm and kill and almost every person who was harmed or killed by
COVID-19 suffered this fate because their immune system was weakened
and overly inflammatory due to inadequate 25(OH)D. None of these
diseases, and very little sepsis, will occur to people who are vitamin D
replete, by the proper standard of 50 ng/mL (125 nmol/L).
#08-misinf
8 The
UK government misinforms the public about the adequacy of fixed,
excessively small, supplemental intakes of vitamin D3 and about intakes
greater than 0.1mg 4000 IU / day being potentially harmful
Misinformation will surely be Word of the Year for 2022.
Here are some examples of the UK government
misinforming
the public about vitamin D, and so about a crucial nutrient nearly all
people lack, with serious, pervasive, negative impacts on their health
and happiness.
There's no mention of the immune system.
. . . there is currently not enough evidence to support taking vitamin D solely to prevent or treat COVID-19.
This is at odds with a great deal of evidence. Hundreds of studies are analysed with great care at:
https://vdmeta.com, which now features the Quraishi et al. 2014 graph.
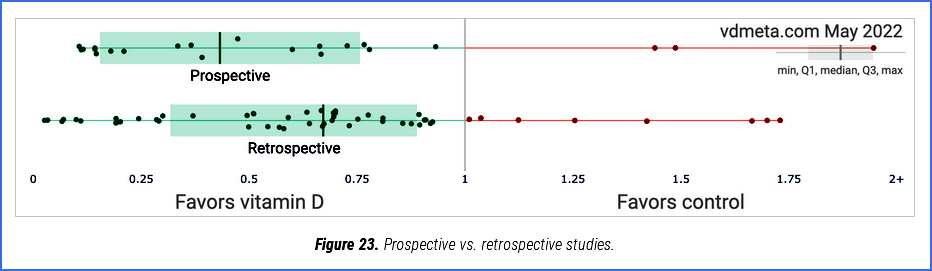
From about late March/early April to the end of September, most people
should be able to make all the vitamin D they need from sunlight.
This is obviously not the case, since most Britons make the most of the
sunlight which reaches the UK, and their vitamin D levels are generally
terribly low. It wouldn't help much to tow England to somewhere
off the coast of Spain, since the Spaniards' 25(OH)D levels are not
much better. (Leave the Scots to their low-elevation sunlight and
trust they heed Dr Helga Rhein's advice at
ScotsNeedVitaminD.com.)
If the NHS was operating as a fully integrated health service, this
vitamin D page which talks up direct skin exposure to the sun would
surely link to another one:
However, the final sentence of the vitamin D page does warn about skin
damage and cancer from being "out in the sun for long periods".
It would be helpful to state that vitamin D production in any given day
reaches its maximum - at least in people with white skin - when the
UV-B exposure is about 1/3 of the
erythemal dose.
One erythemal dose of UV-B is the amount it takes to turn the skin
somewhat red. Beyond 1/3 of this, no extra vitamin D3 will be
produced. See:
Determining
an Effective UV Radiation Exposure Time for Vitamin D Synthesis in the
Skin Without Risk to Health: Simplified Estimations from UV Observations
Masaatsu Miyauchi and Hideaki Nakajima
Photochemistry and Photobiology 2016-10-18
onlinelibrary.wiley.com/doi/10.1111/php.12651
Everyone is advised to take 0.01 mg
400 IU vitamin D3 a day, at least in autumn and winter.
Anyone who enquires into the matter knows that this is totally
inadequate. Here is a graph from some recent research in the UK,
showing the distribution of individual subject's 25(OH)D levels at
baseline and after 6 months supplementation with
800 and
3200 IU vitamin D3 a day - 2 and 8 times, respectively, the amount advised by the government.
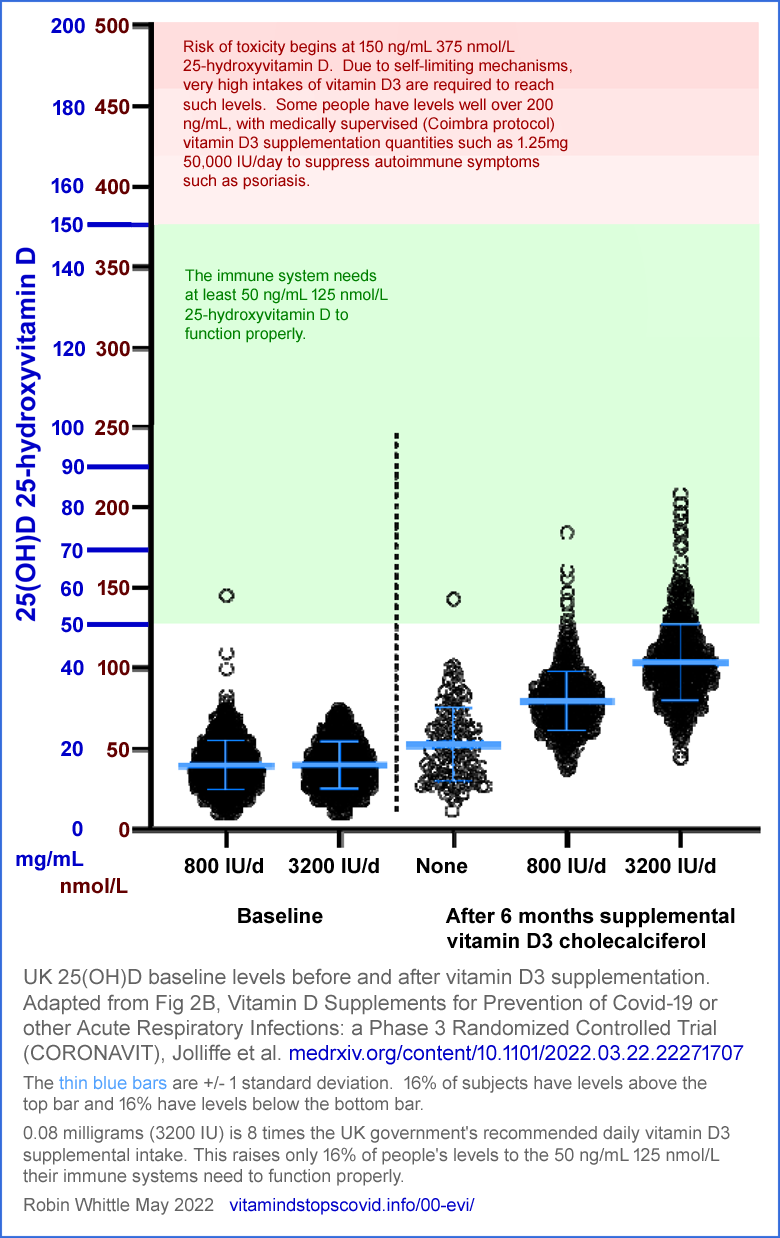
Vitamin
D Supplements for Prevention of Covid-19 or other Acute Respiratory
Infections: a Phase 3 Randomized Controlled Trial (CORONAVIT)
David A.
Jolliffe, 23 others and Adrian R. Martineau
medRxiv (preprint) 2022-03-23
www.medrxiv.org/content/10.1101/2022.03.22.22271707v1
(This RCT had mixed
results. 25(OH)D levels take months to rise significantly with
these small to moderate vitamin D3 intakes - and infections were
recorded while the levels were rising. What really matters is
severe infections which were not recorded. The actual number of
infections, as detected by PCR tests may not be affected much by good
25(OH)D levels. Good levels will probably lead to infection with
few or no symptoms, and a lasting, broad immunity against the same or
related strains.)
While the 800 IU a day intake did appreciably raise 25(OH)D from the
very low mean baseline of about 17 ng/mL (42 nmol/L), and take most
subject's levels above the far too low official threshold of
sufficiency (20 ng/mL 50 nmol/L) almost none of them attained the 50 ng/mL (125
nmol/L) needed for good immune system health.
Even 8 x the NHS recommended vitamin D intake only raised 16% of subjects to 25 nmol/L 50 ng/mL
The NHS's 400 IU recommendation is probably reasonably effective only
by their 20 ng/mL (50 nmol/L) 25(OH)D sufficiency threshold, which is 40% of what is
required for good immune system health.
The Quraishi et al. 2014 graph at the start of this submission
shows
that immune system weakness at this 50 nmol/L level of 25(OH)D results
in 22% or
so risks of both hospital acquired and surgical site infection, which
is 9 times the risks which result from 50 ng/mL (125 nmol/L) or more.
Tesco has bottles of
90 x 500 IU
vitamin D3 tablets for £3.50. This does not seem excessively
expensive: £14 a year for one person to marginally exceed the NHS
recommended quantity.
However, over 80 years, it adds up to a non-trivial £1040. This
would probably be a bucket full of tablets, all for about £0.72 worth
of vitamin D3, weighing 0.365 grams (22 grains of jasmine rice) for an
entire lifetime. This is a lot of fuss and expense to marginally
improve bone health, while suffering lifelong weakening of the immune
system, with high risk of excessive inflammation, except to the extent
that sun exposure in summer raises the 25(OH)D level appreciably for a
few months.
This 4000 IU figure harms and kills people. A doctor told me off
a few years ago for taking 4000 IU a day. Now that I know more about
vitamin D I take 1.25 mg 50,000 IU a week. Since I guess my
25(OH)D level is probably between 50 and 100 ng/mL (125 and 250 nmol/L)
I am happy. I haven't bothered to get it tested, and I haven't
needed to go to the doctor since except for a checkup.
The UK government is simply copying the IOM's 4000 IU upper limit
figure, and scaring its citizens and doctors unnecessarily about the
risks of vitamin D toxicity. This is 25% more than the 3200
IU/day intake in the Jolliffe et al. graph above, and not a single
subject had their 25(OH)D level more than halfway to the level at which
toxicity begins to become a concern. (See the Endocrine Society
Guidance above.
#es)
Another rough estimate of the long-term vitamin D intake quantities
which might cause toxicity can be found in the observations of:
Safety
Data in Patients with Autoimmune Diseases during Treatment with High
Doses of Vitamin D3 According to the Coimbra Protocol
Ulrich
Amon, Raul Yaguboglu, Madeleine Ennis, Michael F. Holick and Julian Amon
Nutrients 2022-03-06
www.mdpi.com/2072-6643/14/8/1575
Medically supervised patients used much higher vitamin D intakes than
are usually required to suppress a variety of inflammatory autoimmune
diseases. Average vitamin D3 intakes were
1.32 mg 52,955 IU a day for patients
suffering from
MS (multiple sclerosis) and
0.742 mg 29,683 IU a day for
patients suffering from rheumatoid arthritis, psoriatic arthritis,
connective tissue diseases, plaque psoriasis, inflammatory bowel
diseases and autoimmune inflammation of the thyroid gland.
These doctors were not particularly concerned about 25(OH)D levels and
did not mandate testing. However, for those patients whose
25(OH)D levels were tested by their own doctors, the average level was
141.4 ng/mL (353 nmol/L). This put less than half of them above a level at which toxicity might be a concern.
This mean of 141 ng/mL of Amon et al.'s patients is about 3.5 times the
40 ng/mL mean of Jolliffe et al.'s 3200 IU intervention group.
Yet Amon et al.'s patients were taking, on average, very approximately
12 times 3200 IU / day.
This demonstrates the general effectiveness of the body's 25(OH)D self-limiting mechanism.
The Amon et al. patients taking, very approximately, 40,000 IU/day
would be at some risk of toxicity in the absence of other nutrients,
dietary restrictions and the medical care they were receiving.
However, the IOM/NHS upper limit of 4000 IU is far too low. For
70 kg non-obese people, the Endocrine Society's 10,000 IU upper limit
is surely safe, since it must be crafted to apply also to adults of 50
kg or so.
By portraying the outdated and discredited IOM upper limit as a real
threshold of toxicity, the UK government further suppresses the will
and ability of UK doctors and members of the public to supplement the
quantity of vitamin D3 they need for good immune system health.
I recall a story in one of the English newspapers in 2020, of a London
taxi driver who spent months in hospital with severe COVID-19. He
eventually recovered. I recall he was a Pakistani or Bangladeshi
Briton. His wife was quoted as stating, with sadness and
puzzlement, something along the lines of:
"But he had been taking vitamin D."
He probably had been - at the UK government recommended daily quantity
which adds up to the mass of a grain of jasmine rice every four years.
Imagine the plight of a psychotherapist, trying to help her patient - a highly regarded barrister - who has been watching
Robert Malone MD and
Pierre Kory MD interviews on YouTube and so came to believe that there is outright
corruption and
regulatory capture
of the United States health, food and drug administrations. He
then came to believe that much the same has happened in his native United
Kingdom, albeit in a more genteel manner.
His life and work is in disarray because he feels compelled to sue the
UK government for something akin to false advertising. The law is
well established regarding making false claims about one's products and
services. He plans to turn this law against the government,
and have them found guilty of falsely portraying a competitor's
products as shoddy, not fit for purpose, or at least not fit to be used in
any quantity which would enable them to be effective.
She listens to his persuasive explanations that the denigrated product
- vitamin D - competes not with the government's own product, but with
the vastly more expensive and profitable products of the multinational
pharmaceutical companies (patented drugs, "vaccines" and monoclonal
antibodies) - and that it is these companies' pernicious, corrupting,
influence which has transformed the operation of whole government
departments, year after year, into doing their bidding. While
pervasive corruption was much less brash than in the USA, he is
convinced of the merits of his case and is driven to discover all the
sordid details so he can argue his case assiduously in court.
Given the divergence of the abovementioned NHS page from readily
ascertainable facts, what chance does the psychotherapist have of
convincing her client that the government's vitamin D advice is
truthful - based soundly on what we have come to refer to as "the
science" - and that it is Drs Malone and Kory and dozens of others who
are in the grip of, and so unknowingly promulgating,
misinformation and
conspiracy theories?
This would be good material for a fantastical thriller screenplay if
the barrister's conception of reality was not so close to our everyday
experience.
#09-role
9 The best ways governments can support their citizens regarding vitamin D
Briefly:
- Governments must not mandate, nudge
or unreasonably cajole their employees or members of the public
to take any nutritional supplement or to accept any medical
intervention or invasive test.
- Governments should not make nutritional supplements or drugs, or
have them made specifically for them. The public should be able
to choose from the commercial products of competing companies regarding
food, nutritional supplements, drugs and all other medical treatments.
- In the case of vitamin D at least, the UK government should set
standards for stability, purity, accuracy of contents and labeling of
tablets, capsules and drops, certifying suppliers, including via
regular testing, so the public can be assured that such products on
sale in the UK are safe and effective if used as directed.
- The government may purchase such products for use in its
hospital, medical centres, aged care homes and prisons, but the staff
and residents there should always be offered the choice between suitable
products and never expected to use any of them.
- Similarly, the government may purchase or subsidise the purchase of
vitamin D supplements to encourage their adoption among sectors of
society who might benefit from such assistance.
- The government must never
try to suppress debate about nutrition, health, medicine - or anything
else. To do so not only reduces the ability of people to make
well-informed decisions, but causes many people, perfectly reasonably,
to loose trust in the government.
- The government should work with knowledgeable vitamin D
researchers, many of whom are doctors with decades of experience, to
develop the best approach to encouraging the public to regard regular
vitamin D supplementation as a relatively simple, inexpensive, but very
important aspect of their nutrition and health.
This will not be difficult, considering the crucial importance of good
25(OH)D levels, but great resistance can be expected from multinational
pharmaceutical companies whose products will be needed less once most
people's immune system functions properly.
It is the government's responsibility to facilitate the best
environment in which citizens can care for their own health. This
requires an environment of free debate about competing theories,
research efforts and the effectiveness of multiple products and
protocols.
Attempts to find the best approach by stifling debate and curtailing
the ability of doctors to communicate freely will result in distrust
not just of the government, but of nutritional supplements it promotes,
even if the supplements are in fact the best approach to improving
health and happiness.
#10-sjw-bio
10 Sunil J. Wimalawansa's bio and July 2022 article
Sunil Wimalawansa, MD, PhD, MBA, DSc., in New Jersey, USA, is the former Head and an Emeritus Professor of Medicine,
Endocrinology & Nutrition at Robert Wood Johnson (RWJ) Medical
School (now merged with Rutgers University) and RWJ University Hospital,
New Brunswick, New Jersey, USA.
He was previously tenured Professor of General Medicine &
Endocrinology at the University of Texas Medical Branch at Galveston
(1993-2001) and earlier, Senior Lecturer/Consultant physician in
Clinical Medicine, Chemical Pathology & Endocrinology at Royal
Postgraduate Medical School (RPMS) & Hammersmith Hospital in
London, UK (1982-1992).
Resume:
https://www.ama-assn.org/system/files/2019-03/bio-sketch-sunil-wimalawansa_0.pdf
He has been researching vitamin D scientifically since 1984 and clinically since 1996.
His most recent article covers many of the topics discussed above:
Update history
2022-05-15: Initial version of this
page, not public, but used to generate the Word and PDF file we sent to
the Office of Health Improvement & Disparities.
2022-05-17: Explanatory header and new sections 7, 8 and 9 added.
2022-05-21: Links added to Key
points section. Page made public.
2022-05-26: In Key points, corrected "1.75 mg" to 0.175 mg for 7000 IU.
2022-06-06: Thanks
to notes and suggestions from Robert
Lutey, corrected numerous typos and expression errors. Added the
calcifediol patent graph, which was not part of the submission
submitted by deadline.
2022-07-09:
Fixed typos. In section 2.2, regarding granulomatous disorders
such as sarcoidosis, added a reference to Kamphuis et al. 2014.
In section 6, several updates: 1 - Link to I-PREVENT and I-RECOVER Long
Haul COVID protocols; 2 - Added two charts depicting the ranges of
ratios; 3 - No evidence for lower ratios for underweight body type; 4
Mechanisms by which obesity reduces 25(OH)D levels.
2022-09-18:
Linked to Prof. Sunil Wimalawansa's article and included a table of his
ratio of body weight recommendations for vitamin D supplemental intake.
2022-09-21: Made a separate section #4.7 for the use of calcifediol to boost 25-hydroxyvitamin D levels in 4 hours.
2022-11-18: Corrected an extra zero at the top left of the graphs at #charts and added a note that Prof. Wimalawansa's later recommendations in his Nutrients article #sjw-updated-ratios are somewhat different.
2022-12-05:
Added the URL for the PDF of Quraishi et al. 2014. Noted that the
Australian fortaro.com site was no longer working. Added material
to Section 3.2 on in-utero neurodevelopment, regarding autism,
intellectual disability, ADHD and schizophrenia. Added a new
section 3.3 on Parkinson's disease and related diseases.
2023-06-03: Added link at the start to the Brownstone.org
article. Removed links to Word files of updated submission.
Added a link to and discussion of Sandboge et al. 2023
#sandboge in the section
#3.2 section "The damage begins in-utero". Added three dot points at the start.
2023-10-02: This is a
significant revision. The state of this page up to this date can be seen at:
web.archive.org/web/20230928105510/https://vitamindstopscovid.info/00-evi/ (This will show a 2022-05-29 version until archive.org update their system.)
The changes were:
- Minor changes in some sections.
- Renamed the page from "Vitamin D: UK Call for Evidence Submission
from Robin Whittle and Patrick Chambers MD" to "Vitamin D and the
Immune System - How much vitamin D3 to take, by body weight and obesity
status". While the page was written as a submission to a UK
government enquiry, they never received it.
- Streamlined initial material.
- Added a new first subsection - the first real subsection after
the link to Dror et al. 2022 and the infographic which depicts its
results - to cover Prof. Wimalawansa's simplified recommendations for
vitamin D3 supplemental intakes as ranges of ratios of body weight,
with higher ratios for those suffering from obesity. This
includes two graphs of body weight and vitamin D3 supplemental
quantities.
- Revised the section on how these ratios were developed: #06-ratios, to include a timeline of the various ranges or ratios.
- Altered all the text, including some quoted text, to represent
25-hydroxyvitamin D levels primarily as ng/mL with nmol/L figures in
brackets.
2024-06-08: Minor corrections and improvements, early explanation
of autocrine vs. intracrine signaling. Added a link to Life
Extension vitamin D3, K and iodine capsules.
2024-09-13: I had incorrect IU / kg values in
#00-how-much. I gave the mcg /
pound figures as mcg / kg, and did not have mcg / pound figures.)
2024-11-25: Added link from the pregnancy and chidbirth section to new Substack article.
© 2022 to 2024 Robin Whittle, Daylesford, Victoria,
Australia. Please reproduce sections with full
attribution to https://vitamindstopscovid/00-evi/
. Do not copy the entire document to any public website. Please refer to this site,
since there will no-doubt be corrections and other improvements.
Sub-sections, such as 2.1, can be linked to with targets, such as https://vitamindstopscovid.info/00-evi/#2.1 . Made with Fabien Cazenave's Kompozer 0.8b3.