Vitamin D3 supplemental intake as a ratio of bodyweight - for
people of all ages. (The suggestion of an electronic technician.)
The page below, and its sub-directories a-ratios/ and b-grh/
are as they were on 12 December 2020, 5 weeks after I first made these
pages. While there may be items of interest, including the
analysis of the Grassroots Health vitamin D calculator's behaviour, the
most important material below is covered better in several sections of
a page which is a May 2022 submission to a UK government department's
request for evidence regarding vitamin D.
Please see the sections:
Vitamin D3 supplemental intake quantities as a ratio of bodyweight with three ranges of ratios:
70 to 100 IU / day per kg bodyweight. Under-, normal- and over-weight.
100 to 150 IU / day per kg bodyweight for those suffering from obesity.
150 to 200 IU / day per kg bodyweight for those suffering from morbid obesity.
These are based on and extrapolated from the ratios used by Afshar et al. 2020.
The completely false IOM (Institute of Medicine) vitamin D recommendations:
- 20 ng/mL 50 nmol/L 25-hydroxyvitamin 25(OH)D supposedly signifies sufficient vitamin D.
- 0.015 mg 600 IU vitamin D3 a day (RDA) is supposedly enough for adults to attain this.
The articles which show the RDA calculation, even for this low 25(OH)D should have resulted in an RDA of about 7000 IU.
Articles from 2006 onwards calling for about 50 ng/mL 125 nmol/L being the proper minimum level of 25-hydroxyvitamin D.
Generally, please refer to the above sections in preference to the following pages.
Robin Whittle rw@firstpr.com.au 12 December 2020
(First established 2020-11-08. 25OHD calcifediol patent graph infographic updated 2021-02-23. )
To the main page
These ratios are intended to be authoritative recommendations, but
they are not peer-reviewed or, yet, supported by any MDs or researchers - however, some MDs in Dubai recommend similar ratios
You are reading something written by an electronic technician, as a suggestion for what would be the best
way of advising people on how much vitamin D to supplement, as a ratio
of bodyweight.
This is a fundamentally different way of recommending vitamin D
supplementation levels from the age-based frameworks normally employed
by governments and professional organisations, such as the Endocrine
Society.
This suggestion, or something along these lines - if accepted by
nutritionists, MDs, researchers and health authorities - would
replace complex existing
conventions with simple guidance which will work well for all people, in
all nations, whose bodies are all shapes and sizes - from newborns to
the elderly.
The text below is written as a draft of what I imagine an authoritative nutritional
recommendation would be. If you are a nutritionist, doctor, nurse or
researcher and would like to fully or partially support what I suggest
here, please let me know, since I would really appreciate this.
Until and unless some such qualified professionals state publicly that
they partly or fully support what follows, please remember that you are
reading the
best efforts of an
electronic technician in the important field of human nutrition.
Please see links to research on obesity and COVID-19:
https://aminotheory.com/cv19/obesity/ and the latest research:
https://aminotheory.com/cv19/#lr .
The details of how I derived these ratios from the work of Ekwaru et al. 2014 are on a separate page:
I did this before I became aware of the Grassroots Health vitamin D calculator or the work of
Parviz Afshar and colleagues:
#grh
There is a
ratio-based vitamin D calculator at Grassroots Health:
A second page here analyzes the output of this calculator:
The Grassroots Health calculator's base and upper ratios seem to be:
1.35
to 3.6
micrograms of D3 per kilogram bodyweight per day.
with rounding up or down to the nearest 25 micrograms = 1000 IU
AND with maximum quantity = 0.25mg = 250 micrograms = 10,000 IU. |
A Grassroots Health
chart states that for a population of people with an unsupplemented 25OHD level of
20ng/ml, supplementary D3 of 69 IU per kg bodyweight will raise their 25OHD levels so that 90% of them attain at least
40ng/ml. This is
1.725 micrograms of D3 per kilogram bodyweight per day.
#2020-Afshar
Iranian MDs at a hospital in Dubai, UAE have been using
ratio-based
vitamin D3 supplemental quantities since 2010 with some opthalmology
patients, and, with great success since early June 2020 with all their
COVID-19 patients.
1.75
to 2.5
micrograms of D3
per kilogram bodyweight per day.
70 to 100 IU/kg/day.
0.8 to 1.14
micrograms of D3 per pound bodyweight per day.
32 to 46 IU/lb/day. |
Without supplementation, 95% of their patients had 25OHD levels below
35ng/ml.
With their ratio-based D3 intakes, and 7.2mg 300,000 IU bolus initial
D3 doses, all 500 or so patients over multiple years attained at least
40ng/ml and none more than
79ng/ml. There was no toxicity, which is to be expected, since toxicity only becomes a concern over 150ng/ml (Endocrine Society
guidelines 2011, still current).
They also suggest simplified arrangement for people whose bodyweight is
between 50kg 110lb and 100kg 220lb: 1.25mg 50,000 IU D3 a week.
This is
0.178mg 7143 IU D3/day =
3.56 to
1.78 micrograms of D3 per kg bodyweight per day.
We cannot over-emphasize the role of Vitamin D in
controlling all infectious diseases especially in COVID-19.
We had no patients with initial Vitamin D levels of
>40ng/ml that required more than 2 to 3 days of
hospitalization, hence no cytokine storm, hypercoagulation,
nor complement deregulation occurred.
Prior to this change, we had several deaths of COVID-19
patients on respirators.
. . . we would like to propose changing
the vitamin D level to 40 to 100-ng/ml as normal [they mean healthy] and consider below 40ng/ml as
deficient.
A section below
#iom discusses how the Institute of Medicine (IOM), in 2010
and 2011, completely miscalculated the Recommended Daily Allowance of
D3 for 25OHD levels of
20ng/ml,
and how - despite this failure, which has never been corrected - the IOM
recommendations from those years are still the foundation for most
government vitamin D supplementation recommendations.
#ratios
The ratios I derived from Ekwaru et al. 2014 and the notes which go with them
My suggestion for the core
recommendation text is in this light grey box. Some other notes and graphs
follow.
The next section has some additional notes, including about how
ratio-based recommendations such as these differ from existing
approaches to recommending vitamin D supplemental
levels.
|
|
There
are two pairs of ratios, one for people with normal and overweight body types and a
second pair for people suffering from obesity. The first ratio of each pair is
the base ratio and the second is the upper ratio.
For people
with normal and overweight body types:
1.8
to 3.6
micrograms of D3 per kilogram bodyweight per day.
72 to 144 IU/kg/day.
0.82 to 1.65
micrograms of D3 per pound bodyweight per day.
33 to 66 IU/lb/day.
|
Thus, an
average weight (70kg, 154lb)
Caucasian adult's base supplemental intake
is 0.125
milligrams (5000 IU) a day and their upper recommended intake is
0.25mg (10,000 IU) a day. (The average bodyweight [WP] of
Asians is generally less than this, so less vitamin D3 would be
required for an average weight Asian adult.)
For people suffering from obesity:
2.5
to 5.0
micrograms of D3
per kilogram bodyweight per day. 100 to 200 IU/kg/day.
1.14 to 2.28
micrograms of D3 per pound bodyweight per day.
46 to 92 IU/lb/day.
|
Morbidly obese
people should seek medical care and probably supplement with higher
ratios.
BMI is not the best indication of obesity, which it overestimates in
tall people. In order to correctly identify obesity in children,
and
to avoid wrongly classifying tall overweight people, obesity
should be determined by medical examination, waist circumference or
other
recognized methods suitable for children and adolescents.
The
base and upper ratios provide a range of supplemental quantities which
are all safe and beneficial. Since the ratios are based on observations
of people who had some high elevation sun exposure, generally white
skin and some level of vitamin D3 in food and multivitamins, people who
have little or no high elevation sun exposure and/or who have dark skin
and/or who not eat oily fish or take multivitamins would be well
advised to choose a ratio somewhat above the base ratio. The same
applies to overweight people who border on an obese diagnosis:
choose a base ratio closer to 2.5 micrograms/kg/day than 1.8ug/kg/day.
People with reduced fat absorption - such as resulting from Roux-en-Y
gastric bypass surgery or other conditions - should initially double
the D3 supplemental intakes specified above and seek medical advice
based on blood tests to ensure their long-term vitamin D sufficiency.
People whose ultraviolet B skin exposure generates significant vitamin
D may require less than these intakes. However, these upper
recommended intakes, even with high levels of sun exposure, are a third
or less of quantities which might, after many months, lead to risk of
toxicity.
These recommendations apply to all people without acute medical
conditions – newborns to the elderly – except that infants
substantially breastfed by vitamin D replete mothers need no
supplements.
People
with a variety of immune system diseases may benefit from vitamin D
intakes in excess of those suggested above, including intakes which
would cause toxicity in some people. This should be done under
medical guidance, such according to the The Coimbra Protocol for multiple sclerosis. Leading vitamin D researcher Michael Holick reports that 25
ug/kg/day (1000 IU/kg/day) was "remarkably effective in controlling
and/or improving symptoms and improving MRI findings in five MS patients
who either failed to respond to or refused conventional MS
therapy." The patients strive for a "zero calcium" diet and
attain 25OHD levels in the 200 to 300 ng/ml range (500 to 700nmol/L)
without hypercalcemia: https://www.mdpi.com/2072-6643/12/7/2097 .
Vitamin D3 interacts minimally with other nutrients. Taking D3
supplements towards the end of a meal may be a good approach, since this
maximises the time the D3 spends in the upper small intestine, where
fat absorption is most effective.
#sarc
Vitamin D
supplementation may be contraindicated in some rare lymphomas and in
granulomatous illnesses such as sarcoidosis. Medical
supervision and guidance on vitamin D supplementation is necessary for
both conditions, perhaps with supplemental vitamin K2 and with
reference to research which indicates that sarcoidosis patients do
better with vitamin D and calcium supplements:
|
|
According to my interpretation of the Ekwaru et al. 2014 article
from which I derived these ratios, a population supplementing
with
base intake quantities will raise their 25OHD levels to an average of about
50ng/ml, with half the people having levels below this. The
upper supplementation levels will achieve average levels of about
60ng/ml, with only a small proportion of people having levels below
30ng/ml.
The subjects of the Ekwaru research all, to some degree or other,
gained D3 from UVB skin exposure, food and probably multivitamins which
were not included in the formal supplemental values reported.
These intakes were not calculated by the researchers, but were
presumably typical of the Canadian adult population. Strictly
speaking, the ratios I derived are applicable only to people who also
have similar such sources of D3. However, these intakes are
small compared to the intakes the ratios recommend. So the ratios
should work well even for people who have very little other sources of
D3.
Today, many governments are contemplating COVID-19 vaccinations for the
majority of their populations, with lockdowns, social distancing and
other unsustainable suppression measures continuing well into 2021.
Similarly comprehensive, voluntary, vitamin D repletion using these ratios will be far
less expensive and much safer than vaccination, with no need for medical
staff, complex administration or visits to remote areas. It will
also be far more effective against COVID-19 and have numerous other health benefits. This is nutritional
support, not a drug or medical intervention.
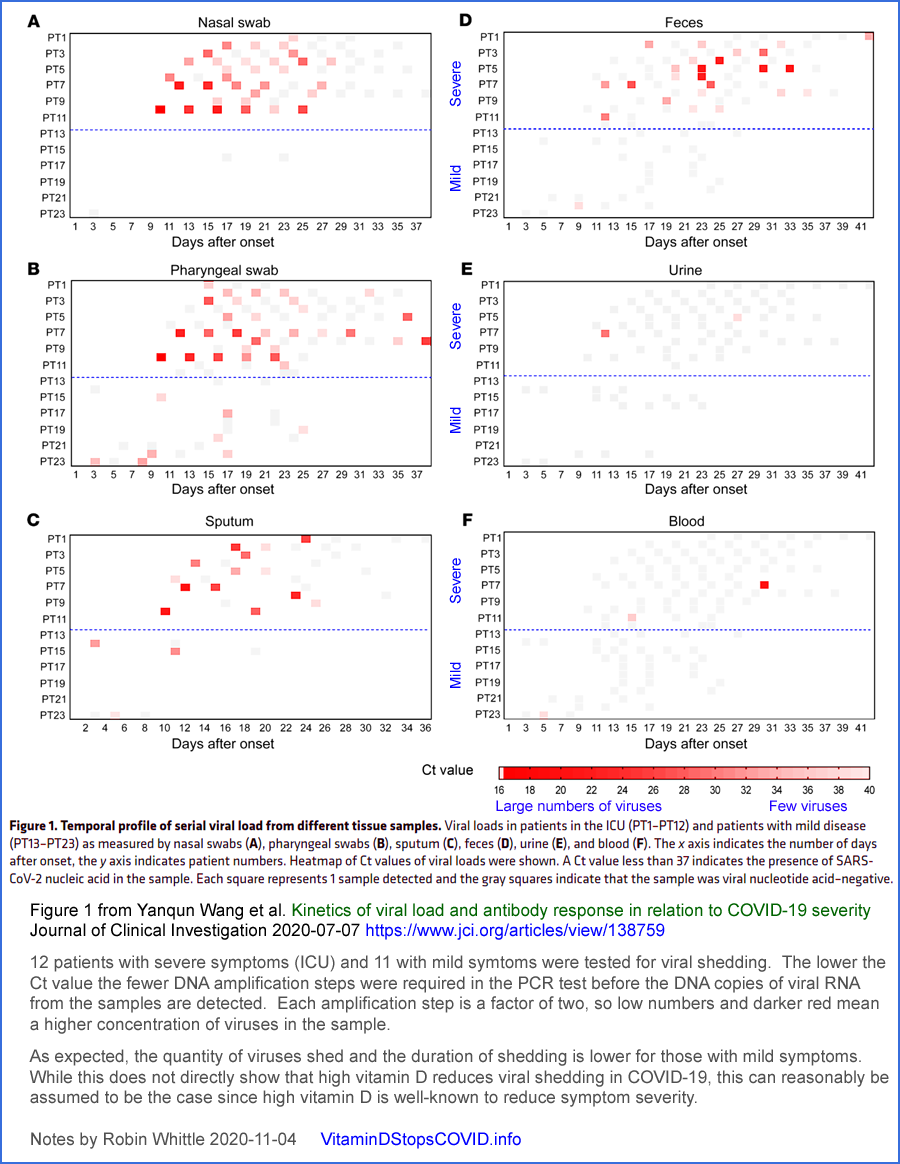
COVID-19 severity, viral shedding and transmission
Please see the
main page for infographics and links to research on vitamin D and COVID19.
Vitamin D replete individuals - those with
40ng/ml or more 25OHD - have a somewhat reduced chance of
coronavirus infection for any given viral insult.
If infected,
their symptoms will be greatly reduced and the risk of lasting harm and
death will be a small fraction of what would be with unsupplemented
25OHD levels. More importantly still,
vitamin D replete people
who are infected will shed viruses for fewer days, and in much smaller
quantities than those who are not.
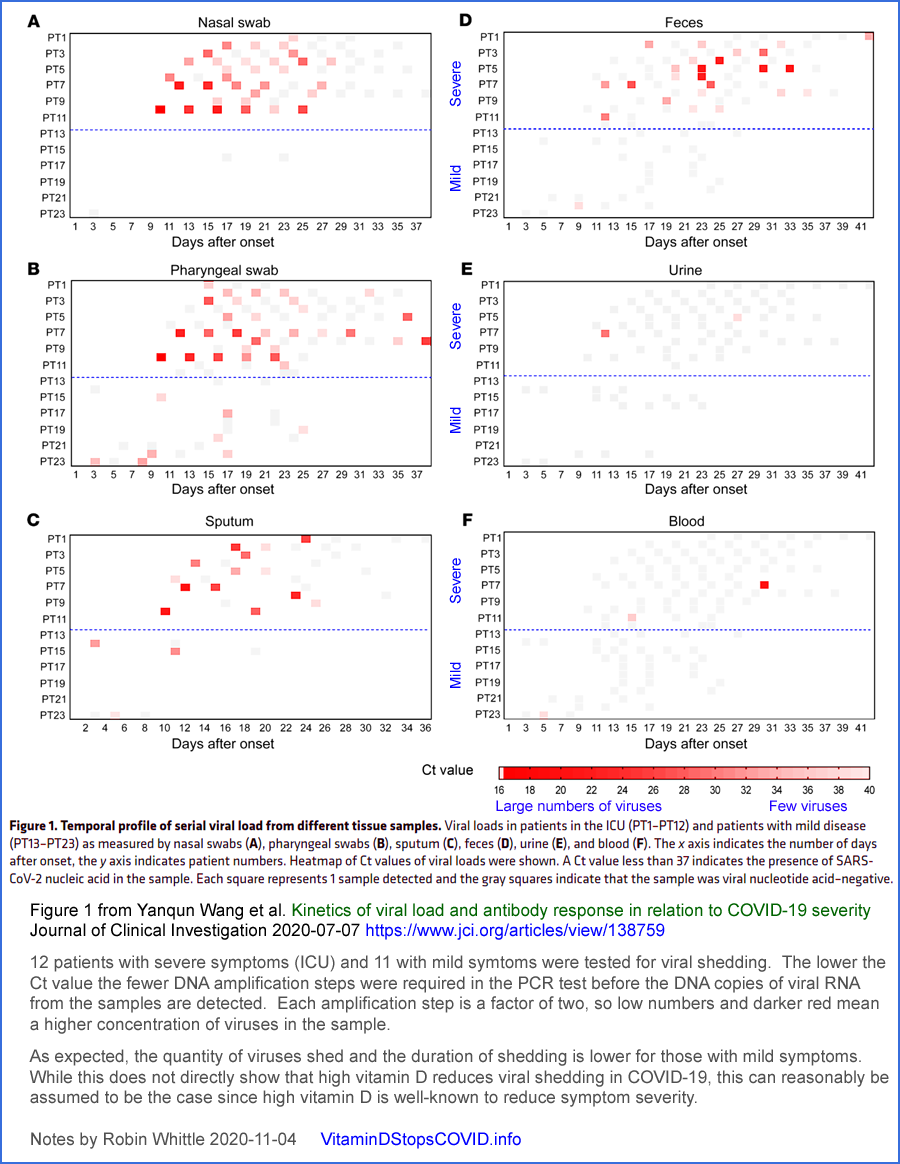
(Adapted from Figure 1 of
https://www.jci.org/articles/view/138759 .)
This last effect is the most significant for ending the pandemic, and the most important in terms of personal responsibility.
Population-wide vitamin D repletion
aiming at average vitamin D 25OHD levels of around 50ng/ml (125nmol/L)
will quell COVID-19 transmission and end the pandemic, in all seasons,
without lockdowns, social distancing or masks.
The summer average 25OHD levels of UK
white people is around 24ng/ml. This is sufficient to greatly
suppress the transmission and symptom severity of both COVID-19 and
influenza. So it is reasonable to assume that
population-wide supplementation to achieve average 25OHD levels twice
this will result in very low rates of transmission all year round, and
similarly low risk of severe symptoms for those few who are affected -
for both COVID-19 and influenza.
Furthermore, this approximately
50ng/ml average level of 25OHD will suppress transmission no matter how
the current hundreds of strains of SARS-CoV-2 and influenza continue to
mutate.
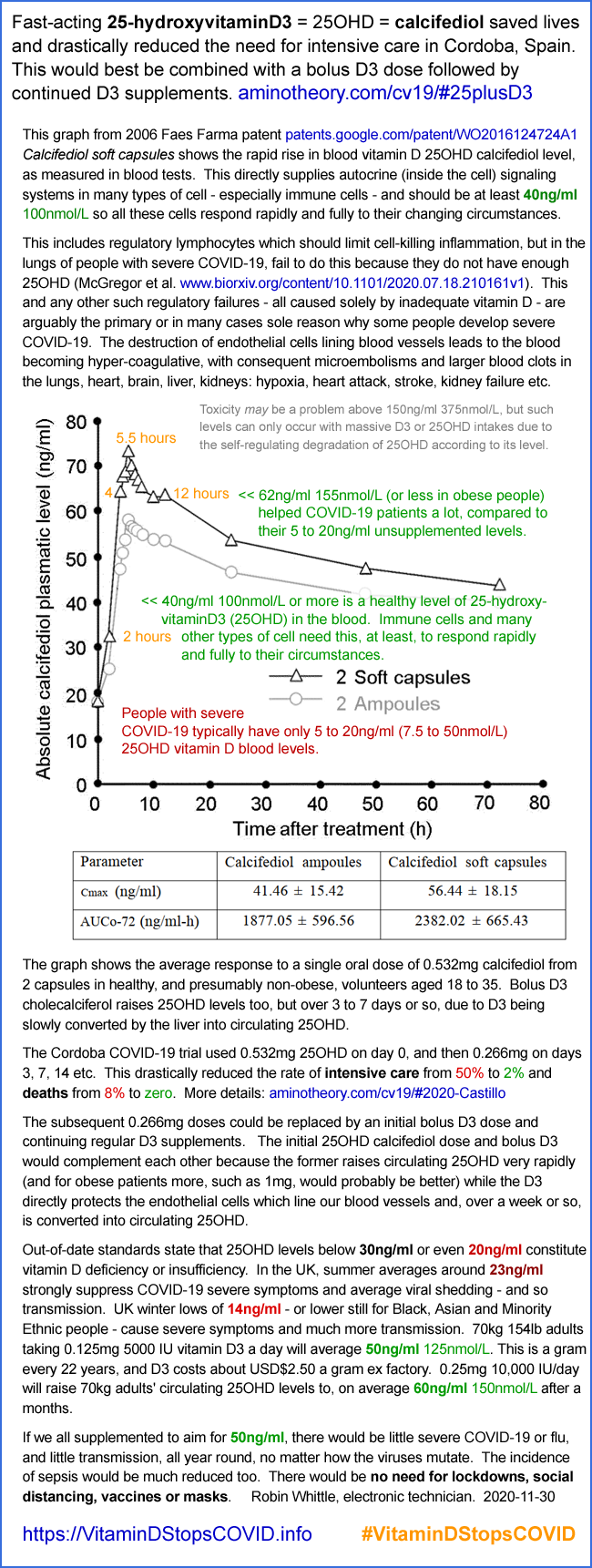
#25plusD3
25plusD3 - my suggestion for a D3 & 25OHD calcifediol
combination supplementation treatment for COVID-19, severe influenza
and sepsis
This is a terse account of the fuller proposal at
https://aminotheory.com/cv19/#25plusD3
, for immediate adoption in the current COVID-19 crisis, and also for
severe or potentially severe influenza as well as for
sepsis. Here I discuss my suggested
25plusD3
protocol in the future context of the population generally robustly
supplementing D3 to attain healthy, ca. 50ng/ml 25OHD vitamin D levels.
This is a suggestion for treating severe or
potentially severe COVID-19 in light of the resounding success of the
Cordoba 0.532mg oral 25OHD calcifediol trial (Castillo et al. 2020 -
see links and discussion at my other website:
https://aminotheory.com/cv19/#2020-Castillo and the link and discussion below) and in the light of the success of earlier trials of bolus oral D3.
In the generally high (average 50ng/ml 25OHD) vitamin D future I
propose, those few people who suffer serious COVID-19 symptoms can be
treated with the MATH+ protocol [
https://covid19criticalcare.com],
plus a loading dose (bolus dose) of D3 and 0.5mg to 1.0mg so of 25OHD calcifediol to
achieve much more rapid and complete recoveries than are achieved in
many hospitals today.
Effect
of Calcifediol Treatment and best Available Therapy versus best
Available Therapy on Intensive Care Unit Admission and Mortality Among
Patients Hospitalized for COVID-19: A Pilot Randomized Clinical study
Marta
Entrenas Castillo et al. Journal of Steroid
Biochemistry and Molecular Biology
https://www.sciencedirect.com/science/article/pii/S0960076020302764
|
Of the Cordoba trial's 26 control patients, 13 (50%) needed intensive care
and 2 (7.7%) died. Of the 50 patients who received 25OHD calcifediol, 1
(2%) required intensive care and none died.
A bolus dose of, for instance 12.5mg (500,000 IU) D3 over 5 days would take several
days to to a week to raise 25OHD levels on its own, but will
sustain these levels for a few weeks at least. So an initial
0.5mg 25OHD calcifediol dose and a bolus D3 dose, both at the earliest
opportunity, will raise 25OHD within hours and for the next few
weeks. The D3 itself, without conversion in the liver to 25OHD,
directly stabilises the endothelial cells which line the blood
vessels [
Gibson et al. 2015]
- the destruction of which in severe COVID-19 causes the
hypercoagulative state of the blood, which causes microembolisms and
larger blood clots in all organs.
My
25plusD3 suggestion will only be a bona-fide protocol after some MDs adopt it.
There is an urgent need for better treatment of severe or potentially severe COVID-1. There is no time or need for
RCTs etc. People are being harmed and are dying all over the
world right now, and one doesn't have to do a lot of research reading
to conclude reliably that both components of what I propose: ~0.5mg to 1.0mg
25OHD AND a robust bolus dose of D3, both at the
earliest opportunity
are safe and beneficial. The two complement each other very well,
as I discuss in the abovementioned section at my other website.
As of mid-November 2020, Cordoba-style Co25OHD dosing OR bolus D3 are
part of the MATH+ protocol. I believe they should both be used
together, but this is a most welcome development. Full details at
https://aminotheory.com/cv19/#25plusD3 . See also:
https://aminotheory.com/cv19/#calcifediol-availability .
More on severity, shedding, transmission and other similarities between COVID-19 and influenza
The same principles of reduced severity, shedding and transmission apply also to influenza: with average 25OHD levels of
50ng/ml,
the flu virus will hardly spread at any
time of year due to low viral shedding - and would rarely cause
serious harm. Those few with severe symptoms could be treated
much better than at present with the D3 and 25OHD (combination
cholecalciferol and calcifediol therapy) as just described. There
would be no need for flu vaccines.
SARS-CoV-2 / COVID-19 and influenza share a striking similarity in the
degree to which their symptom severity and transmission rate
(presumably largely due to viral shedding rates) rise in the winter and
spring period for countries far from the equator. In India, the hot, wet, cloudy monsoon [
WP],
keeps most people indoors and out of direct sunshine. Vitamin D
levels drop, COVID-19 surges and with the end of the approximately June
to September monsoon this year, new COVID-19 case numbers which had
been rising to mid-September, have since (to early November) been dropping just as rapidly as they rose:
https://ourworldindata.org/coronavirus/country/india?country=~IND .
(See also: Implications of Monsoon Season & UVB Radiation for COVID-19 in India Rahul KM, Lennart Kraft medRxiv .)
Both of these observations can be reliably assumed to be
due mainly or wholly due to the decline in vitamin D levels caused by
reduced direct high-elevation sun exposure. There is little
evidence linking seasonality of influenza or COVID-19 to temperature,
humidity or behavioural changes, though these and numerous other
factors including lockdown, social distancing and masks surely affect the spread of the diseases to some extent.
On this basis it is reasonable to assume that the symptom severity of
both diseases depends very much on the weakened and/or dysregulated
immune responses which naturally occur in all people when they 25OHD
levels are low, well below the
40ng/ml or higher range now recognised as being essential for immune system health.
Another striking similarly between the two diseases is how influenza
severity - and presumably total viral shedding - is driven to a high degree
by obesity, which is now well known (see my page
https://aminotheory.com/cv19/obesity/
which lists risks including lower D3 conversion to 25OHD, and ectopic
ACE2-expressing adipocytes in the alveolar tissue) to be a high
risk condition for those suffering from COVID-19:
Incidence of the extreme immune dysregulation disorder
sepsis
- which according to the following analysis causes 20% of all deaths
worldwide - will be significantly reduced when most of the population
supplements with sufficient vitamin D3 to raise average levels by a
factor of three or four to about
40ng/ml.
Sepsis, severe COVID-19 and severe influenza all involve extreme levels
of immune dysregulation. Likewise the childhood and adolescent
conditions Kawasaki disease and Multisystem Inflammatory Syndrome:
https://aminotheory.com/cv19/#2015-Stagi .)
The success of the Cordoba calcifediol
trial can reasonably be extrapolated to the prospect of treating sepsis, KD and MIS
patients with similar oral calcifediol amounts to raise their 25OHD and
so improve autocrine signaling and immune system regulation within a
few hours.
Evidence for the effectiveness of substantial bolus D3 doses in sepsis
comes from a 2015 RCT in which a 12.5mg (500,000 IU) D3 bolus dose over five
days halved the average length of hospital stay from 36 days for the
control group to 18 days for this supplementation group. This
supplementation raised the average baseline 25OHD level from 20 to
53ng/ml on day 7. Half the amount of D3 over five days
reduced the average hospital stay to 24 days:
High dose vitamin D administration in ventilated intensive care unit patients: A pilot double blind randomized controlled trial
Jenny E Han et al. Journal of Clinical & Translational Endocrinology 2016-05-05
https://doi.org/10.1016/j.jcte.2016.04.004
|
Numerous other chronic and acute diseases are caused, at least in part,
by chronic inflammation. These conditions include both types of
diabetes, auto-immune conditions and neurodegenerative disorders
including Alzheimer's and Parkinson's diseases. These and other
diseases involving chronic inflammation can be expected to become less
prevalent with the end of the Vitamin D Deficiency Pandemic.
Vitamin D need not be taken every day, so larger supplemental intakes
every 5, 7 or 10 days are as effective as daily intakes. As mentioned above, D3
itself, without conversion to 25OHD, stabilizes endothelial cells
throughout the body. This relatively recent discovery implies
that
the interval between D3 capsules should be no longer than a week or
so. Longer intervals between supplemental intakes would probably
allow liver conversion of D3 to to substantially deplete the
circulating D3
which endothelial cells depend upon.
Prioritizing those most in need in a time of crisis and the urgent need for new vitamin D3 cholecalciferol factories
Engineers do not debate the merits of
fully charged batteries, or of tanks filled with uncontaminated
fuel. It is standard practice to supplement indoor-housed
agricultural animals with nutrients, including vitamin D3.
Arnold L. Hirsch describes vitamin D3 production in his 2011 book chapter Industrial Aspects of Vitamin D.
In 2010, 77 tonnes of less refined D3 was manufactured for agricultural feed
and 20 tonnes in a highly purified form for human consumption.
Today, pharma-grade D3 costs about USD$2,500 per kilogram ex-factory,
for instance
this AliBaba seller. In November 2020 I learned, from an
interview
with Satish Verma, MD of Fermenta Biotech in India, that approximately
35 tonnes of pharmaceutical grade D3 is produced per year, for human
food fortification and for supplements such as capsules and drops for
infants. Approximately 4 times this D3 is also produced, in a
less refined form, for agricultural animal feed.
Depending on levels of obesity, full adoption of the above recommended
D3 intakes would lead to average daily intakes of about 1/6000 of a
gram per person per
day. This is about 60kg per million people per annum,
reflecting
the fact that humans need about one part per million body weight of D3
per year. At current prices the required pharma grade D3 would
cost USD$150,000 per annum per million people. Since this
would save hundreds of millions or perhaps billions of dollars worth of
health costs per year, this represents an astronomically high return on
investment.
Most D3 production is in China and India. The output of those
factories is insufficient for the needs of these countries'
people. So all countries with the capacity to do so should build
D3 factories with utmost haste. I can't rule out innovative
techniques, but unfortunately it probably takes at least a year to
build a D3 cholecalciferol factory using established
techniques. So I think that for the northern winter of late
2020 and early 2021, we are going to have to draw down stocks of human
D3 and use some animal feed D3, which is generally made into a spray
dried powder form with 1.25% D3. I assume that this is
perfectly fine for humans, since it is fine for the animals we eat.
The starting compound is cholesterol, extracted from wool fat.
This is converted in several steps to high purity 7-dehydrocholesterol,
which is then dissolved in a hydrocarbon solvent.
Special kilowatt sized mercury vapor lamps
with iron doping are required
to produce the precise ~297nm UVB wavelengths which are required.
The hydrocarbon solvents used for the
reaction and purification steps are largely recycled but the process is
onerous, since the solvents are volatile, highly inflammable and there
are multiple stages of distillation to recover the D3 from the other
compounds present.
In the initial stages of the country-wide programs which would
eliminate most or all of the serious threats posed by both COVID-19 and
influenza, vitamin D3 will be in short supply, so the recommended
intakes will not be achieved for all people until new factories are
operational.
During this time it would be best to recommend full daily intakes and
perhaps loading
doses up to 60 days equivalent for the people in greatest need,
starting with all hospital patients and healthcare workers. These
people include residents and staff of aged care homes and of
correctional facilities, police, emergency service workers and the
armed forces. Transport workers and those whose work is most
critical to governments and utilities would come next. The
elderly and those with black or brown skin should also be prioritized
since they are most likely to have low levels of D3 production in their
skin.
These recommended D3 intake ratios are easily applied to all people, of
all countries, without reliance on medical resources. They
supersede existing guidelines, which typically set a particular intake
for broad groups of people, such as those aged 1 to 17.
Production and distribution of D3 capsules and drops for infants, with
clear multi-lingual guidance on correct dosage, should be left to the
private sector so people can choose the products which most suit them.
Governments should support D3 repletion with multilingual information
for the public, healthcare workers and pharmacists. Limits on
per-capsule quantities, such as 0.025mg (1000IU) in Australia,
should
be lifted so average weight people can purchase capsules which match
the weekly quantities recommended above, such as for a 90kg person
using 2.7ug/kg per day: 1.7mg (68,000IU).
With mass production of smaller numbers of higher capacity capsules,
there is great scope for reducing the annual cost per person of D3
supplements. For instance, at present, in Australia, with
five 1000IU capsules a day, the annual cost for an average weight adult
using the
base ratio, using the
least expensive
capsules available is ( (365 * 5) / 400) = 4.6 bottles @ AUD$14 each =
AUD$64.40 per annum. This is good value, but involves five
capsules a day, when one a week would be more convenient and less
expensive. The total amount of D3 in this year's supply at 0.125mg
(5000 IU) a day is 0.046 grams, which has an ex-factory cost of about
US 12 cents, or AUD$0.17.
The public should be informed and reassured that the recommended
intakes are safe and beneficial and that there is no reason to exceed
these intakes except under medical advice.
25OHD testing is unavailable in many parts of the world.
There is
no need to test the blood vitamin D levels of healthy people in any country. The cost
and medical effort such tests involve would be better directed to other
health and nutrition needs. The supplemental D3 quantities
described above support the levels of an essential nutrient
which is very well researched and known to have large safety margin
between the amounts required for good health and those higher amounts
which might, for some people, result in toxicity.
The above is a suggested way of specifying nutritional support,
which involves no medical supervision or testing, because it it is not
medicine, and does not involve drugs or their risks.
There are other common nutritional deficiencies which deserve concerted
government effort to correct. Zinc deficiency has been implicated
as a causal factor in severe COVID-19:
https://www.medscape.com/viewarticle/938793 .
Omega 3 fatty acids, vitamin C, B vitamins (especially B12 for older
people) and iron all deserve such attention. Please see Hira Shakoor et al. 2020-08-14:
Be well: A potential role for vitamin B in COVID-19. Vitamin K2 is found
in many foods, but its deficiency has been implicated in COVID-19
severity (
Simon Goddek 2020-08-04). It is vital for calcium-bone metabolism and coagulation
regulation. Adequate vitamin K2 is thought to reduce the risks of
hypercalcemia from greatly excessive D3 supplementation.
These other nutrients are worthy of investment regarding research,
education and population-scale repletion. However, none of them
come close to vitamin D, which is needed by so many cell types, in such
small quantities, and for which global repletion would constitute a
profound revolution in human health.
How these bodyweight ratio D3 supplemental suggestions differ from conventional ways of recommending
vitamin D supplementation
Governments and other organisations which make recommendations for
vitamin D supplemental intake quantities do not, as far as I know,
define those quantities as a ratio of bodyweight - even though this is
the simplest form such recommendations could take while remaining
applicable to all people. An exception is Grassroots
Health, who use ratios in their calculator and in an intake
recommendation chart mentioned above #grh.
As far as I know, all these government recommendations make specific quantity recommendations,
such as for a basic intake and a maximum safe intake, according to
classes of people in which the population is divided into categories
by age and other characteristics.
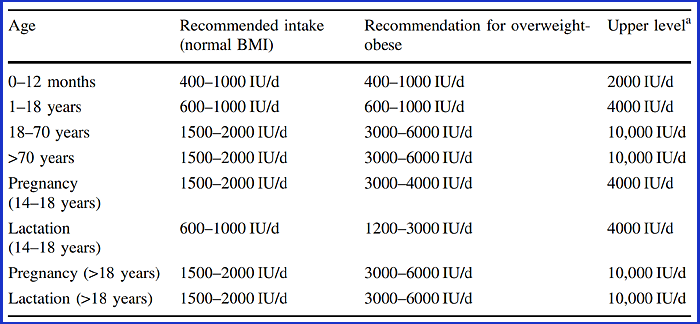
This is exemplified by the following table which attempts to generalize
the divisions and quantities used by most developed nations.
Many countries base their guidelines on the fatally flawed 2011 work of
the US IOM (as discussed below
#iom). The IOM's
calculated RDA for vitamin D was less a tenth of the correct
figure. Their RDA figure of 0.125mg (600 IU) is all through their
recommendation table, and is used by the USA and many other
countries.
The UK government recommends only 0.01mg (400IU for adults).
This tiny quantity is approximately the mass of 2mm of human hair - a
gram every 274 years - less than one UK pence worth of vitamin D
per year.
These conventional approaches (now referring to the generalised table above the IOM one) are inferior to the ratio of bodyweight
approach I suggest above in several ways:
- The quantities are generally too low - and at times
disastrously low, such as for 17 year olds, and worse still
for obese 17 year olds.
- Age is used as a proxy for body weight.
- People are binned into broad categories according to age,
despite the great range of body weights in each category.
- The 16 first and second column categories plus 8 upper level
columns are overly fussy and not needed.
- The maximum level takes no account of obesity.
The suggestions above explicitly state that D3 supplementation is
nutritional support, not a medical intervention or anything to do with medicine at all.
The suggestions above also specifically state that
25OHD testing is not required
for the general population and furthermore, even when it might be
possible to test a significant proportion of the population, that this
not be done so that the resources can be used for a better purpose.
This
no mass testing aspect of the suggestions above are are, as far as I know,
novel. This may seem radical considering that many doctors today
prefer to regularly test their patient's 25OHD, and that a number of
new vitamin D promotion schemes, developed or revamped this year due to
the COVID-19 crisis, explicitly require initial and perhaps regular
testing. These include:
In order to achieve a very high degree or success in repleting vitamin
D all round the world, the arrangements need to be lightweight,
applicable to all people, and not rely on expensive infrastructure such
as pathology labs which are not available in many countries.
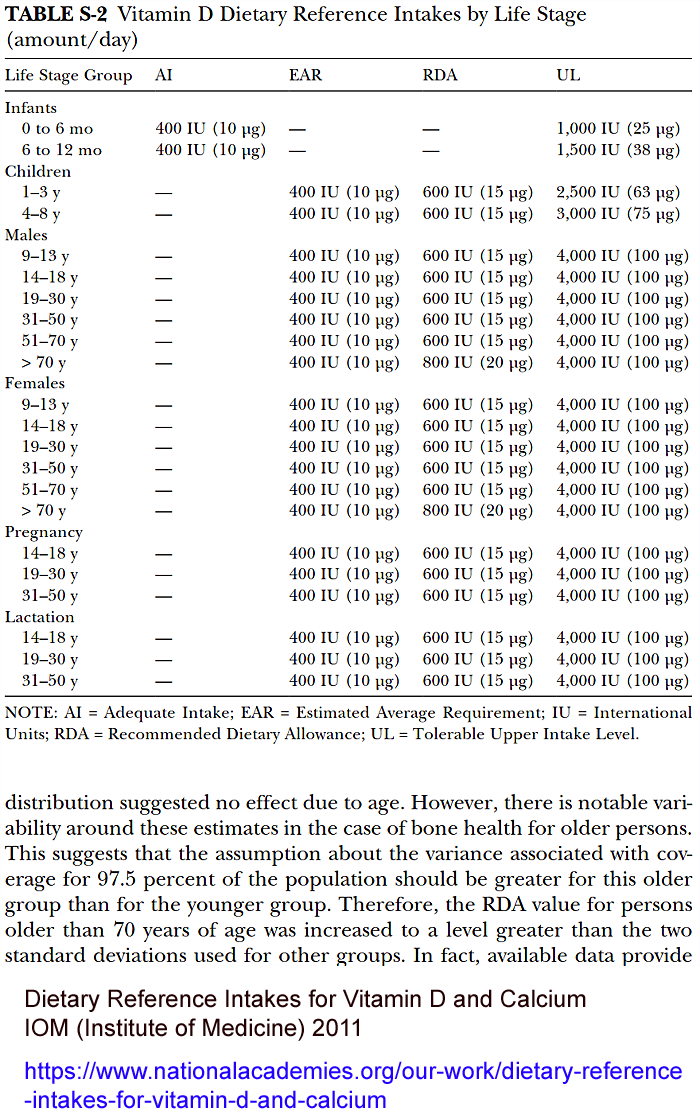
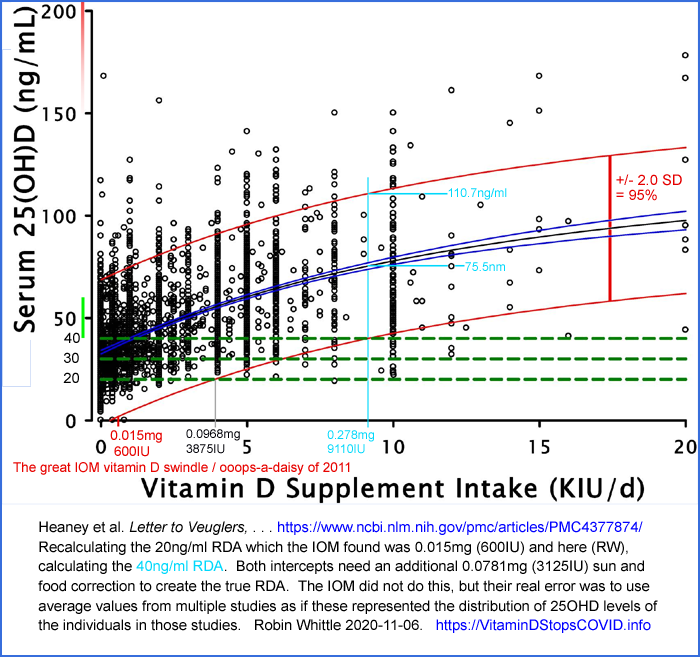
The IOM's great blunder in calculating the 20ng/ml RDA for vitamin
D3 - and why I believe a D3 RDA for achieving 40ng/ml is undesirable
There are a variety of factors holding
back official D3 supplemental quantity recommendations from according
with our current knowledge of the immune system and the role adequate
vitamin D plays in its proper function.
One major problem is that most committees who control such
recommendation documents rely on now-discredited guidance from the US
Institute of Medicine's 1133 page report. A central feature of
this report, and all the other recommendations which arise from it is
that the RDA (Recommended Daily Allowance) for D3 to achieve
20ng/ml
(in at least 97.5% of the population, which is the definition of RDA)
is
0.015mg (600IU).
The fault in the IOM's calculations was first reported by P. J. Veuglers and J. P. Ekwaru in 2014:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4210929/ .
The IOM's blunder was simple and devastating.
In order to find the RDA it is necessary to use the statistical distribution pattern of numerous
individual
25OHD levels which result from one or more different supplementation
quantities. By finding a supplemental intake in which the mean
and the standard deviation ensured that two standard deviations below the
mean resulted in the desired 25OHD level, this ensures that 95% of the
subjects' 25OHD levels were within the +/- 2 SD range of the mean, with
2.5% of the individual levels above the +2SD line and 2.5% below the
-2SD line.
Instead of analysing the individual 25OHD levels and supplemental
intakes of the individual subjects in all the research studies they
were using, the IOM instead analysed the statistics of the averages of
each such study! This distribution of points on the intake vs.
25OHD graph tells
us nothing about the 25OHD levels of the individuals in these
studies. So it is impossible to calculate the RDA in this
way. The IOM used the distribution of average levels of trials as
if they were the individual levels of a small number of actual people.
In March 2015 Robert Heaney and colleagues revisited the IOM's mistake and
performed a proper analysis on their own data set of individual 25OHD
values, for subjects taking a variety of supplemental D3
quantities:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4377874/
They estimated the true 20ng/ml RDA for the cohort on which their dataset was based as:
. . . must be close to 0.175mg 7000 IU per day. . . .
So the IOM's RDA was a factor of 10 or 11 too low.
Robert Heaney and colleague's result was partly due to them correcting
for their subject's D3 inputs from UVB exposure, food and any
supplements not counted by the research study. This was
done by extrapolating the somewhat curved mean line to the horizontal axis which
represents zero 25OHD. This correction, which the IOM did not
attempt, is perfectly valid since the definition of the RDA involves
all D3 inputs, including supplements, food and from UVB exposure.
The IOM's work has never been corrected - and to this day forms the
basis of vitamin D supplementation guidelines in most countries.
So the IOM's RDA
still is a factor of 10 or 11 too low.
This one, simple, statistical error has arguably had extraordinarily
destructive repercussions - though by rights it should have been
acknowledged in 2014/15 and the whole of the IOM's report revised
according to the new knowledge about the
20ng/ml RDA really being about
0.175mg 7000 IU.
If this error had never been made, of if it had been promptly corrected
four years ago, then the IOM's guidance on vitamin D supplementation
would have been very different.
In its 2010 and 2011 deliberations the IOM rebuffed submissions to set its target 25OHD level higher than
20ng/ml on account of the demonstrated importance such higher levels
have for immune function and other "extra skeletal" (not concerning
calcium and bone) aspects of health. The IOM argued against
such evidence and decided to aim for
20ng/ml 25OHD which they, probably
correctly, asserted was sufficient to enable the kidneys to produce the
very much lower levels (a factor of 1,000 or so) of circulating
1,25OHD calcitriol, which functions as a hormone to regulate calcium and bone
metabolism.
Had they chosen a higher target, most likely
30ng/ml, then even with
their conceptual error, they would have arrived at a higher RDA than
0.015mg (600 IU).
If the IOM had correctly calculated the
20ng/ml RDA at about
0.175mg 7000 IU,
it is reasonable to imagine that by now the resulting official
guidelines in many countries would have lead to much greater general
levels of supplementation, and the creation of new factories to meet
the few hundred tonnes per year demand for D3 which this would create.
To the extent that this was actually adopted by most people in a given
country, we would have seen a revolutionary transformation in general
health, with the most dramatic changes including that influenza was
hardly transmitted in any season, with few of those infected being
harmed. Before long the IOM's work would come to the top of the pile for consideration for the Nobel Prize for Medicine!
Note that this correct RDA, even though it is
only for
20ng/ml, would involve daily D3 intakes much the same as would
result from the
base ratio I suggest above. The incidence
of sepsis would by now be greatly reduced. Furthermore,
SARS-CoV-2 would not spread very much and would rarely cause serious
harm.
Can anyone think of a comparable blunder with such far-reaching consequences?
Instead we now have:
- A globally debilitating combination of COVID-19
pandemic and the lockdown measures by which governments attempt to
control it - all for lack of 45mg or so 25OHD a year for 70kg adults.
-
A situation where the UK government sincerely believes
that 0.01mg 400IU is an adequate daily intake of D3 for its citizens,
all of whom live far from the equator. (Though, thanks to input from MPs Rupa Huq, David Davis, scientists and advocates the government is, in November 2020, seeking revised guidance on D3 supplemental intakes.)
-
Many MDs who consider that adults ingesting
more than 0.1mg 4000IU will lead to an unacceptable risk of
toxicity! The real figure is probably 8 times this for average weight adults and 20 times this for obese adults.
I want to highlight this extraordinary blunder because it is not widely
enough known. I only learned about it in October 2020 and I
have been devouring vitamin D research for a year or so.
If anyone thinks my suggested ratios of
1.8 to 3.6ug/kg bodyweight are
too high, they should remember that the resulting amounts for a 70kg
adult: 0.125mg 5000 IU to 0.25ug 10,000 IU are very close to the
20ug/ml RDA which the IOM should have calculated in 2011.
This raises the question of what the RDA would be for what we now regard as a good 25OHD level:
40ng/ml.
Here is my attempt to calculate not exactly the RDA, but something
like
it - without the correction for the subjects' non-supplemental D3
inputs from food and UVB exposure. I did this after deriving the
ratios above from the work of Ekwaru et al. With careful
Photoshop measurements of Heaney et al.'s graph, I found that the
figure was about 0.278mg (9110 IU) - to which 0.0781mg (3125 IU) for
food and other sources should be added to create the true 40ng/ml RDA
(0.356 mg = 14,244 IU) for the subjects whose 25OHD levels are
represented in this dataset.
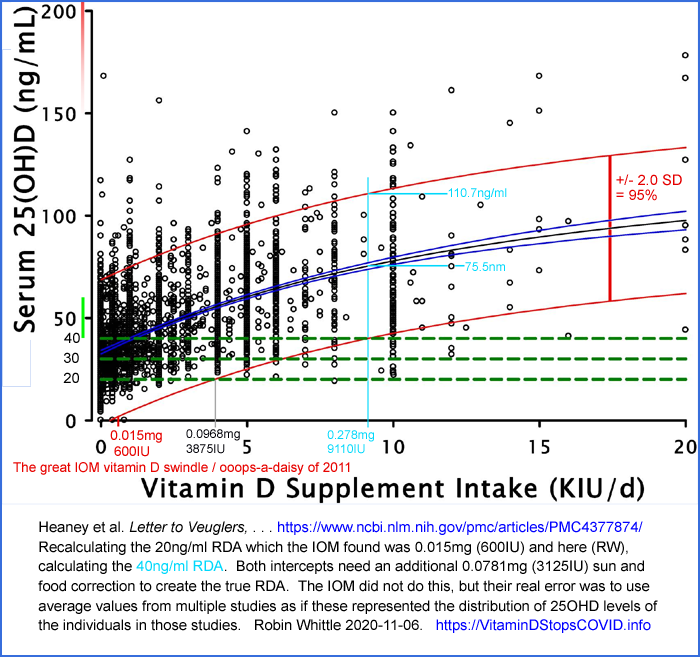
When contemplating this potential 0.278mg (9110 IU) amount as if it
was the amount "all adults" are told to take, I looked at the top red
curve for this intake which is at 110.7ng/ml, predicting that 2.5% of
the population would be above
this. This looks borderline problematic to me, for 70kg adults
because I guess a few of them would have levels above 150ng/ml, which
we are keen to avoid, since it is generally considered the level above
which toxicity may become a problem.
I assume that quite a lot of the high 25OHD
distribution is for people with lower than average bodyweights -
so I don't think we can advocate anything like "adults" taking
this RDA.
Also, the average at this 0.278mg (9110IU) point in the graphs is
75.5ng/ml, which is significantly higher than the 46ng/ml average level
of Luxwolda et al. found for traditionally living Maasai pastoralists and
Hadzabe hunter gatherers.
This line of enquiry lead me to the conclusion that the RDA concept is
fundamentally flawed, at least for vitamin D's 25OHD levels, which
exhibit a great deal of scatter.
The RDA idea is noble. However, with this degree of scatter, the
RDA is forced to be so high that the average 25OHD significantly
exceeds what we observe in populations in which we believe the 25OHD
levels are generally:
46ng/ml.
Part of the scatter is due to the wide bodyweight variation among
adults. This is the primary reason for the RDA concept being
fundamentally broken. There are also questions of body
morphology where excess adipocytes in obese people, from
all accounts,
soak up a lot of the 25OHD and never return it to the
bloodstream - and where the 25-hydroxylase enzyme in the liver is
downregulated, reducing the rate at which D3 is converted to
25OHD. There are numerous other causes of scatter as well,
such as differences in absorption - but researchers have not yet
characterised the various sources of scatter to a satisfactory degree.
I now regard RDA as the wrong approach to nutrition, at least for
vitamin D. Like many concepts whose initial attraction is their
apparent simplicity - such as the BMI formula - the results are a mess
because reality is complex and bad things happen when an unsubtle,
inappropriate, overly-simple rule is applied which would only make
sense if reality was much more constrained than it actually is.
The same thing would happen if it was assumed that multiple clothing
sizes were silly and that what we really need is one size of shirts to
fit everyone, or at least all adults, the world over - or even in one
country.
An RDA calculation ignores 97.5% of the people. It sets an intake
for all people based solely on the 1/40th of the population with the
lowest 25OHD levels. There are numerous reasons for this
variation - body weight is just the most obvious.
So I do not advocate pursuing the RDA for vitamin D.
The ratios I propose will not cause everyone to achieve
40ng/ml. I think we should be happy with what it will
achieve - double to four times the currently parlous 250HD levels of
many people worldwide, with no risk of toxicity.
The Grassroots Health
chart
referred to above is produced by some of the world's foremost vitamin D
researchers. This states that for a population of people
not taking D3 supplements other than multivitamins, who through UVB
exposure, food and any multivitamins attain 25OHD levels of
20ng/ml, then D3 at
1.725 ug/kg bodyweight (69 IU/kg) per day 90% will attain at least
40ng/ml,
This is for a whole population, including an unspecified proportion of
obese people. Many of those who attain less than
40ng/ml will be obese.
The experimental subjects of Ewaku et al. had an unspecified average unsupplemented 25OHD level, I guess in the order of
20ng/ml and my non-obese
base ratio of
1.8 ug/kg bodyweight (72 IU/kg) per day should get more such people over
40ng/ml
than the Grassroots Health ratio, partly because it specifies 4.3% more
D3, but mainly because it applies to people who are not
obese.
The notes in the grey box above, below the ratios themselves, urges
people whose unsupplemented 25OHD levels are likely to be lower than
20ng/ml
to choose a ratio somewhat above the base ratio. A
particular concern is people with pigmented skin living far from the
equator, especially in winter, especially if they cover their bodies
whenever outside.
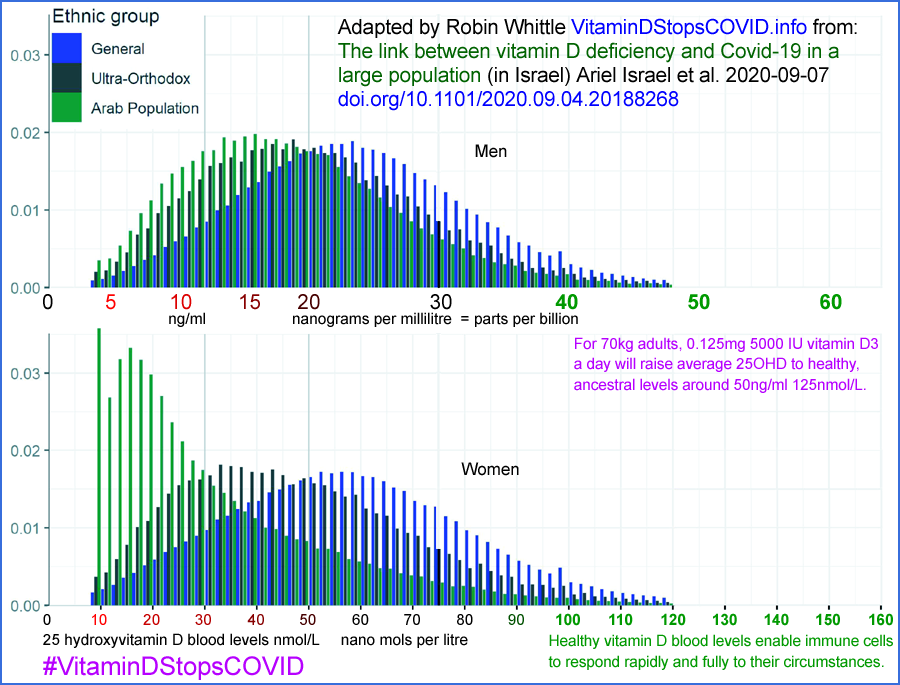
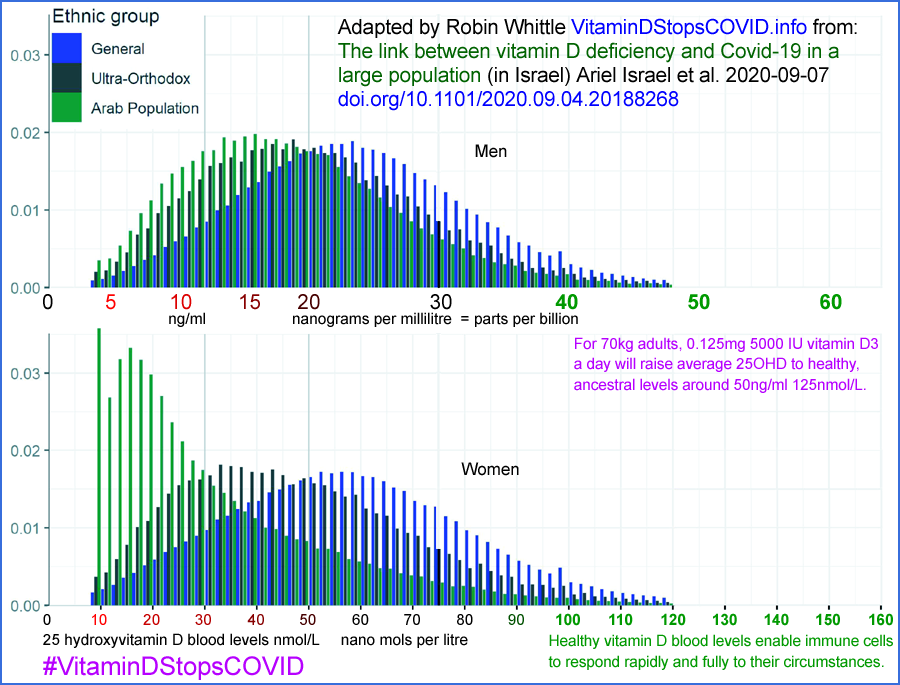
Even in sunny Israel, at 32° north, we see that women who avoid sun
exposure for cultural reasons (Arab - mainly Muslim - women, green on
the bottom), frequently have disastrously low 25OHD levels.
Consider such women living in England, Scotland or Sweden - and their
children.
© 2020 Robin Whittle Daylesford, Victoria, Australia