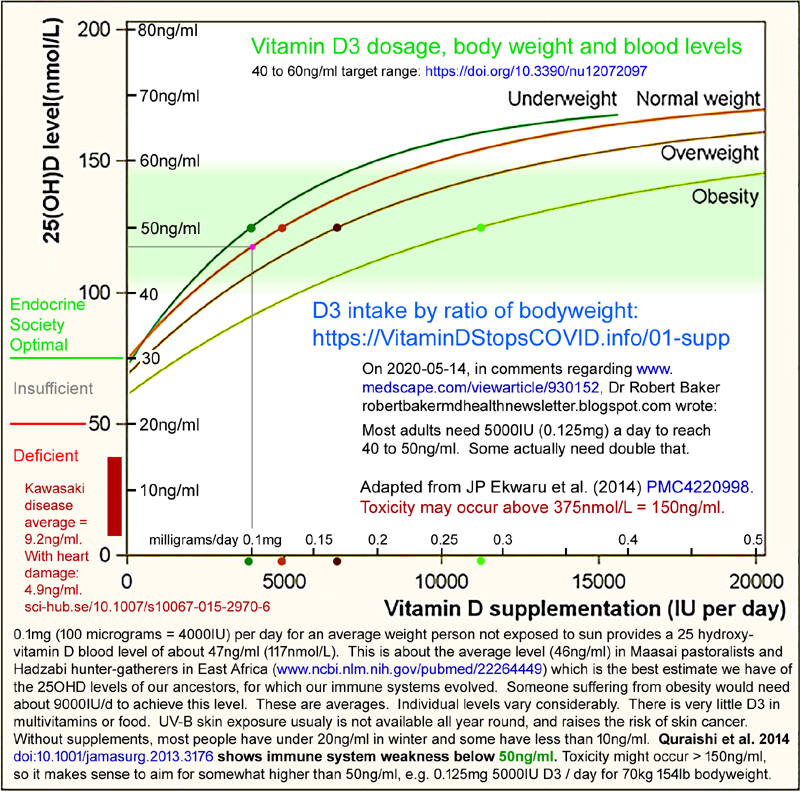
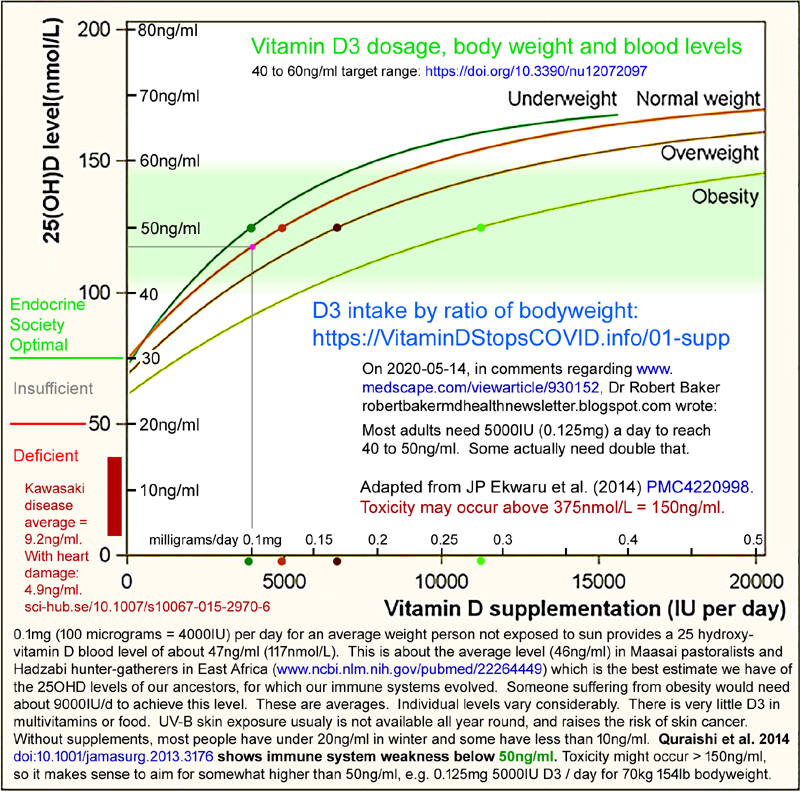
I chose a target, long-term, 25OHD level of 50ng/ml (125nmol/L) because it is in the
middle of the 40 to 60ng/ml
range cited by research articles, the D*Action team
etc. as mentioned in the the 01-supp/
page. Also, Quraishi et al. 2014 showed that levels below
50ng/ml caused weakened innate and adaptive responses against bacterial
pathogens which cause hospital-acquired and surgical site infections: https://vitamindstopscovid.info/02-intracrine/#04-quraishi .
from:
|
The Importance of Body Weight
for the Dose Response Relationship of Oral Vitamin D
Supplementation and Serum 25-Hydroxyvitamin D in Healthy
Volunteers |
These four curves are averages from 22,214 25OHD readings of 17,614
healthy North American adults participating in a preventive health
program. So this is a self-selected sample of the
population. I have assumed a normal bodyweight of 70kg (154lb),
while recognising that normal bodyweights (not average - normal,
healthy, non-overweight, non-obese) bodyweights for Asians are somewhat
less than this.
I used the intercepts of curves and the 50ng/ml 25OHD level directly. I am not trying to develop an RDA. See the end of the 01-supp/ page for my reasoning.
My aim is to get a population of people - whether infants,
children, adolescents or adults - supplementing D3 so the average of
their 25OHD levels is, for the base ratio about 50ng/ml.
Sidebar on RDAs:
This is a completely different approach than trying to derive an RDA to achieve any given 25OHD in a specific subset of people, such as those with a particular bodyweight. To do that we would firstly need to know the distribution of individual readings, ideally for a given supplementation amount, and secondly to add a correction for the fact that all subjects must have gained significant D3 from food, UVB skin exposure and perhaps uncounted multivitamins.
If the subjects had zero such inputs, the curves would all
intersect with both axes.
So the ratios I derive assume some level
of D3 intake from food and/or multivitamins and some level of cutaneous
CD production from UVB exposure. Some people's situations
do not fit the pattern of these study subjects, such as newborns,
infants, women who rarely if ever go outside without full coverage
clothing and the patients, residents and inmates of hospitals, care
homes and prisons. However, the difference between the very
low D3 supplies of these people and those of the study subjects is not
particularly significant in the context of the robust D3
supplementation quantities the chosen ratios will provide.
So we don't need to derive a formal RDA, or estimate the
ex-supplementation D3 supplies of study subjects with any certainty.
To aim for 50ng/ml, according to the Normal Weight curve, 0.125mg (5000IU) is needed, on average. Assuming 70kg body weight this is ratio of 1.8ug/kg body weight. Then there could be different ratios for overweight and obesity.
Ekwaru et al. state (I assume* "1.5 times higher" means the original weight * 1.5, rather than * 2.5):We recommend vitamin D supplementation be 2 to 3 times higher for obese subjects and 1.5 times higher for overweight subjects relative to normal weight subjects.
They mention "two to three times more" in their abstract, citing the Endocrine Society*, and note that their article is intended to provide a research basis to justify this, which the Society acknowledged was lacking.
* They are referring to this article, which remains to this day (Nov
2020) the Endocrine Society's clinical guideline for vitamin D, and which Google reports has
been cited 8,505 times:
This article recommends the IOM's mistaken 600IU RDA for all but those with obesity and those on particular medications. Their terminology regarding higher intakes for those with obesity with is messy too:
[Normal weight] . . . maintenance therapy of 1500 – 2000 IU/d. From their page 1924 restatement of rec. 3.5: 3.5 In obese patients, patients with malabsorption syndromes, and patients on medications affecting vitamin D metabolism, we suggest a higher dose (two to three times higher; at least 6000 –10,000 IU/d) of vitamin D to treat vitamin D deficiency to maintain a 25(OH)D level above 30 ng/ml, followed by maintenance therapy of at least 3000 – 6000 IU/d. They clearly mean 2 * to 3 *. Table 3 shows in the right two columns the Endocrine Society recommendations alongside the sliced and diced arrangement of the IOM, and for adults 19 years and above the daily requirement is 1500 to 2000 IU/d, with 10,000 IU being the "upper level", with nothing about obesity, since this is not an element of the IOM's recommendations. The 1133 page IOM report can be found via www.nationalacademies.org/... . Page 9 (PDF page 26) has their table of recommendations, here as a PNG. An early critique is by Robert Heaney and Michael Holick is at: https://asbmr.onlinelibrary.wiley.com/doi/pdf/10.1002/jbmr.328 . |
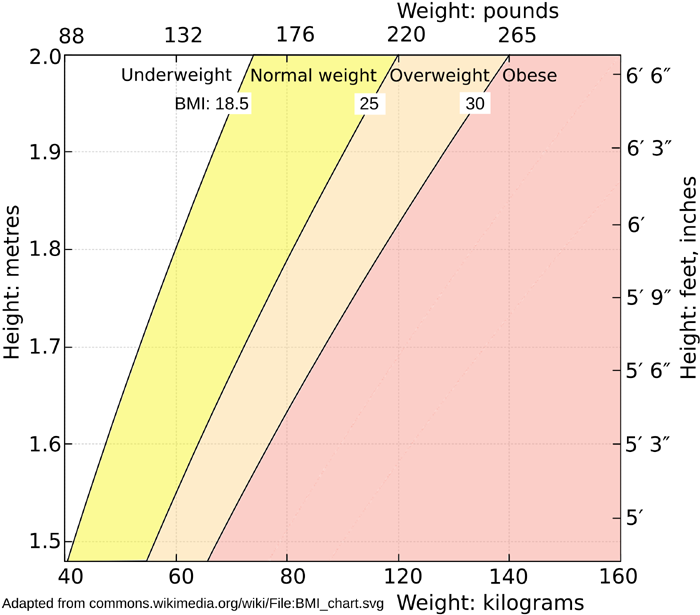
The average BMI of overweight people is 25 to 30 = an average of 27.5, which is 19.25 * 1.425 . So on this basis, we don't need a ratio different from the normal 1.8 ug/kg for the overweight to achieve their goal of 1.5 times the D3 intake of average weight non-overweight people.
Obesity is open ended: BMI > 30. If we take the mid-point
of another step of 5 upwards, this is 32.5 as the low end of
obesity = 19.25 * 1.69 .
To match this with their low end target of 2 times the average weight D3
intake, we need a ratio (2.0 / 1.69) = 1.1834 * the base ratio
of 1.8ug/kg = 2.13g/kg .
I guess that the average high end of obesity is another 5 above this: 37.5 = 19.25 * 1.948. Ekwaru et al. suggest these people need 3 times the average weight D3 intake, so we need a ratio (3.0 / 1.948) = 1,54 * 1.8ug/kg = 2.77ug/kg.
So I chose 1.8ug/kg for normal and overweight people, with 2.5ug/kg for those with obesity, with a note that those suffering from morbid obesity require medical care and probably still higher ratios of D3 per kg body weight.
Since there is such a high safety margin, since some people may
benefit from higher intakes and since aiming for 50ng/ml means
half the people will have less than this, I suggest that these
two ratios: 1.8ug/kg and 2.5ug/kg be the base
recommendation, with upper ratios being twice
these.
There's no research justification for this - but it is
convenient, and has the property of adding about another 10ng/ml
to the resulting average 25OHD levels, as you can see from the curves.
That would match with the widely stated belief - backed up by all observations - that for average weight adults, 0.25mg (10,000IU) is well below an intake where toxicity might be a concern.