Vitamin D and ivermectin cannot reasonably be characterised as "orphan treatments" for protecting against severe COVID-19 and for suppressing disease intensity, viral shedding and so overall rates of community transmission. There is a plethora of evidence for their effectiveness and few, if any, reports of adverse affects when used correctly. Reports of people being harmed by self-administered veterinary ivermectin are a strong argument for MDs being able to prescribe pharma-grade ivermectin.
In addition to the cited work https://covid19criticalcare.com/ivermectin-in-covid-19/ of Paul Marik,
Pierre Kory et al. on ivermectin, the anonymous but professionally
executed meta-analysis site https://ivmmeta.com is a good resource for
people seeking the latest research.
Like ivermectin, vitamin D requires no direct
involvement of medically trained staff and so can scale to whole
populations far more easily than vaccines. Both are inexpensive, very
well researched and protect against all variants of SARS-CoV-2. As an
essential nutrient, vitamin D is more important still. It can best be
obtained through supplementation, since no food contains significant
quantities of it, all-year round UV-B skin irradiation is unavailable to
most people, pigmented skin reduces cutaneous D3 synthesis and all such
UV-B exposure increases the risk of skin cancer.
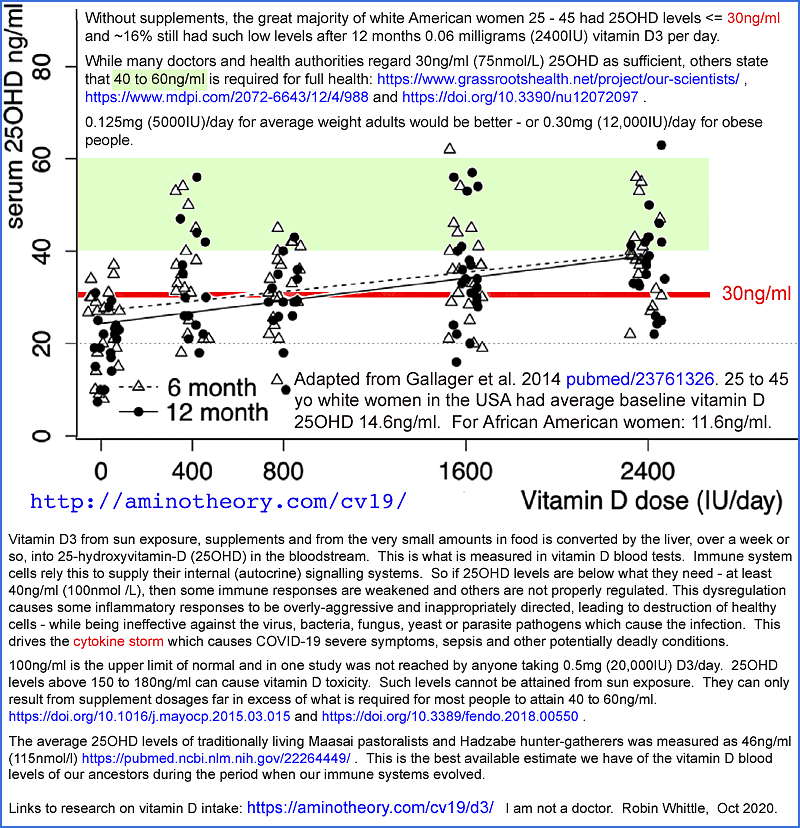
25-hydroxyvitamin D (25OHD) levels such as 20 to
30ng/ml (50 to 75nmol/L) are sufficient for the kidneys to maintain the
very low levels of circulating 1,25-dihydroxyvitamin D (1,25OHD)
required for regulating calcium-bone metabolism. This is the one
hormonal function of the vitamin D compounds and does not affect immune
cells.
Immune cells consume 25OHD when their autocrine
(inside the cell) and paracrine (to nearby cells) signaling systems are
activated[01, 02]. These systems are crucial to the each cell's ability to responds to its changing circumstances.
This locally produced 1,25OHD is not a hormone. It functions as an
autocrine and or paracrine agent, at much higher levels than
circulating, hormonal, 1,25OHD.
It seems that many MDs do not understand vitamin D
autocrine / paracrine signaling and have unreasonable fears of
toxicity[03] when considering the D3 supplemental quantities which are
required, on average, to achieve healthy, ancestral[04 , 05] circulating
25OHD levels of ~50ng/ml (~125nmol/L), such as 0.125mg (5000IU) per day
for 70kg adults[06]. This is a gram every 22 years.
McGregor et al.'s article "An autocrine Vitamin
D-driven Th1 shutdown program can be exploited for COVID-19" [07] is the
most important research on the molecular mechanisms by which inadequate
vitamin D levels drive the pro-inflammatory cytokine storm which causes
some people to develop severe COVID-19[08]. Th1 lymphocytes from the
BALF (Bronchoalveolar lavage fluid WP) of hospitalised COVID-19 patients are stuck in their initial
pro-inflammatory program, and fail to respond to high levels of
complement, which should cause them to switch to their anti-inflammatory
shutdown program. The complement protein is detected and initiates the
vitamin D autocrine signaling system by creating both 1-alpha-hydroxylase enzyme (CYP727B1) and vitamin D receptors (VDRs) in the cytosol.
The enzyme should convert intracellular 25OHD into 1,25OHD,
which binds to the VDR. The bound complex will then migrate to the
nucleus and up- and down-regulate multiple genes, which will cause the
cell to switch to its shutdown program. However, this autocrine
signaling system does not work in these cells, while it does in cells
from the BALF of healthy control subjects. The sole reason for this
potentially deadly failure is inadequate 25OHD.
There has been no direct measurement of the
circulating 25OHD level which, by diffusion to tissues, enables immune
cell autocrine / paracrine signaling to proceed at full speed, to
completion. It is clear from numerous observational and intervention
trial research articles, such as those analysed at https://vdmeta.com,
that higher circulating 25OHD levels are strongly protective against
severe COVID-19 symptoms. High levels properly facilitate autocrine /
paracrine signaling in all immune cells, enabling strong direct
anti-viral innate and adaptive responses, as well as ensuring proper
function of Th1 and other regulatory cells to reduce or eliminate
self-destructive overly-inflammatory responses.
The most direct measurement I am aware of concerns
a large survey of bariatric surgery patients and the relationship
between their pre-operative 25OHD levels and both surgical wound site
infections and other hospital acquired infections[09]. The infection
rates drop precipitously with increasing 25OHD levels and reach their
minimum at 50 to 55ng/ml and above.
Since immune cells' reliance on vitamin D is all through consuming circulating 25OHD to drive their autocrine / paracrine signaling systems, it is reasonable to conclude from this research that 55ng/ml or so is sufficient for all these cells to function well, at least regarding their 25OHD requirements. The fact that these patients were all morbidly obese (the operations were for weight-loss surgery) does not mean the results can necessarily be extrapolated to people not suffering from obesity. However, many people are, so this circa 50ng/ml figure, supported by many researchers, such as this recent review[10], should be regarded as a healthy target for all people, for general health and for protection against severe COVID-19.
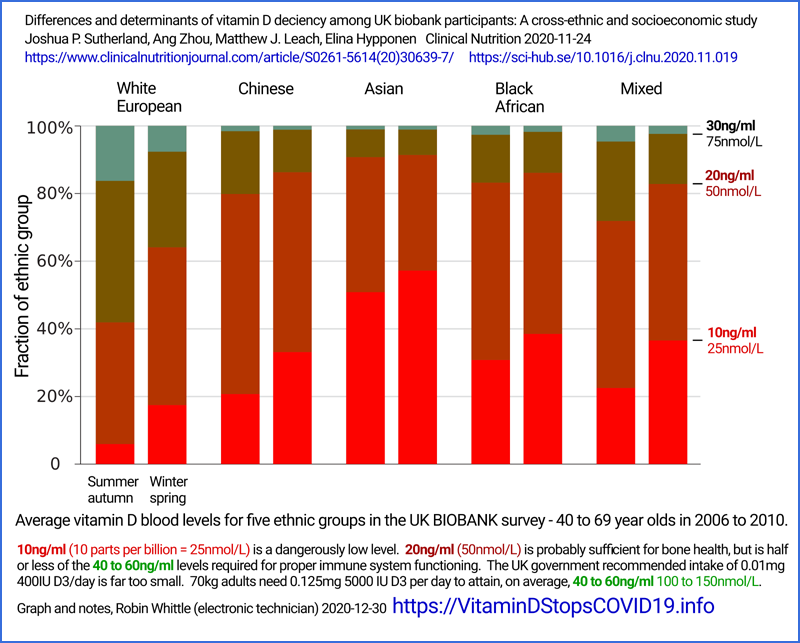
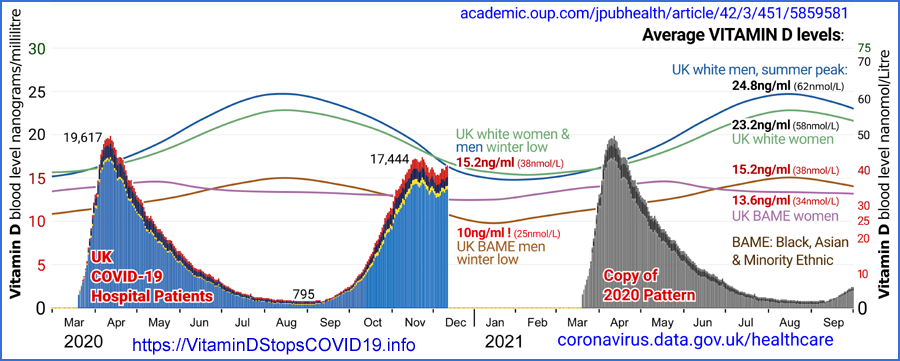
Yet in the UK, most people cannot attain even 30mg/ml in winter, and some never attain it at any time of the year[11, 12, 13].
Higher population average 25OHD levels in the UK summer of 2020 provide the most convincing explanation for the mid-year nadir in COVID-19 infection, hospitalisation and death rates. Summer UV-B also inactivates viruses in outdoor aerosols and on surfaces, but this is unlikely to be a major cause of low R0 since most transmission occurs inside buildings and vehicles. Seasonal temperature and humidity variations are sometimes regarded as important determinants of viral transmission, but the seasonal outdoors variations are typically reversed by heating and air conditioning in the buildings and vehicles in which people spend most of their time in close contact with others.
MDs should be familiar with the 2015 research of
Stagi et al.[14] in which children suffering from the extreme immune
dysregulation condition of Kawasaki disease were found to have average
25OHD levels of 9.2ng/ml. Those with coronary artery abnormalities
averaged only 4.9ng/ml.
Vanegas-Cedillo et al.[15] provide a graph of
COVID-19 death hazard ratio which rises dramatically with lower 25OHD
levels. Tuncay at al.[16] report average 25OHD levels of 36.2ng/ml for
healthy controls, and for COVID-19 patients: 21.2ng/ml non-severe;
14.6ng/ml severe and 10.5ng/ml for those who died.
All the clinical evidence and mechanistic research
points to circulating 25OHD levels below about 50ng/ml being
causatively associated with worse outcomes for COVID-19 and numerous
other conditions. While inflammatory conditions probably do reduce
25OHD levels somewhat - making pre-infection 25OHD levels a more
reliable indication of initial vitamin D sufficiency than those taken
mid-illness - this inflammatory loss of 25OHD is a further argument for
rapid interventions to raise these levels.
Unfortunately, many clinicians first encounter the problems of low vitamin D levels when their patients are already seriously ill or on the brink of becoming so.
In such clinical emergencies vitamin D3
supplementation is of marginal use. Bolus D3 such as several hundred
thousand IU for adults may be helpful, but it takes days to a week or so
for this to be converted in the liver to the circulating 25OHD the
patient's immune cells urgently need.
The only way 25OHD levels can be raised substantially within hours is
with calcifediol, the pharmaceutical name for 25OHD. In the Cordoba
calcifediol RCT of Castillo et al.[17] just 0.532mg oral calcifediol,
given at the earliest opportunity to hospitalised COVID-19 patients,
reduced ICU admissions from 50% to 2% and deaths from 8% to zero. No
25OHD measurements were taken, but the initial rise in 25OHD levels can
be estimated from a graph in a patent for the same Faes Farma Hidroferol
capsules as used in the trial[18]. In young, healthy and presumably
non-obese control subjects, average levels rose from 18ng/ml at baseline
to 63ng/ml or more between 4 and 12 hours after ingestion, dropping
slowly to about 45ng/ml after three days, when follow-up 0.266mg
calcifediol was administered.
Long-term, robust, D3 supplementation is they key to preventing the
worst outcomes of COVID-19 - and likely suppressing viral shedding and
so overall levels of community transmission. However oral calcifediol
may be the closest thing there is to a magic bullet for emergency
COVID-19 intervention, though Pierre Kory et al. report similarly
beneficial effects with ivermectin. Both treatments are effective and
safe, and I am not aware of any reasons why they should not be combined.
The quantity of calcifediol required is very small, and daily D3
supplementation following this should be sufficient to maintain the
raised 25OHD levels. However, calcifediol may be difficult to obtain.
Recently, Dutch nutritional supplement giant DSM released small (150mg)
tablets containing 10mcg in Australia, without need for prescription: https://shop.fortaro.com
. An inexpensive bottle of 60 of these contains about the same amount
of calcifediol as the two capsules which in Cordoba saved many people
from harm and death.
Vitamin D deficiency is recognised as a national problem in sunny
Pakistan, where a Vitamin D Academy has been established[19]. 220 MDs,
PhDs and professors from all over the world signed an Open Letter
calling for all nations to robustly supplement their populations. Most
of these signatories recommended 4000IU/D3 a day and many take more than
this themselves[20]. (They were given the option of recommending 0.05mg 2000IU or 0.1mg 4000IU D3 a day for adults.)
The UK government's 0.01mg 400IU D3 per day recommendation is barely enough to ensure bone health, and a tenth or less of what is needed to properly supply the immune system with 25OHD. This is a gram every 274 years, and D3 costs £2 a gram ex-factory.
01 Hewison M. Antibacterial effects of vitamin D.
Nat Rev Endocrinol 7, 337–345 (2011).
https://doi.org/10.1038/nrendo.2010.226 https://www.nature.com/articles/nrendo.2010.226 (Paywalled.)
https://sci-hub.se/10.1038/nrendo.2010.226
339 Google citations. Discussed at: https://vitamindstopscovid.info/02-autocrine/
02 Whittle R. Vitamin D autocrine signaling - illustrated explanation. https://vitamindstopscovid.info/02-autocrine/
03 Holick MF. Vitamin D Is Not as Toxic as Was Once Thought: A
Historical and an Up-to-Date Perspective. Mayo Clin Proc.nMay
2015;90(5):561-564 https://doi.org/10.1016/j.mayocp.2015.03.015 https://www.mayoclinicproceedings.org/article/S0025-6196(15)00244-X/fulltext
04 Charoenngam N, Holick MF. Immunologic Effects of Vitamin D on Human
Health and Disease. Nutrients. 2020; 12(7):2097.
https://doi.org/10.3390/nu12072097
05 Luxwolda MF, Kuipers RS, Kema IP, Dijck-Brouwer DA, Muskiet FA.
Traditionally living populations in East Africa have a mean serum
25-hydroxyvitamin D concentration of 115 nmol/l. Br J Nutr. 2012 Nov
14;108(9):1557-61. https://doi.org/10.1017/s0007114511007161
06 Ekwaru JP, Zwicker JD, Holick MF, Giovannucci E, Veugelers PJ (2014)
The Importance of Body Weight for the Dose Response Relationship of Oral
Vitamin D Supplementation and Serum 25-Hydroxyvitamin D in Healthy
Volunteers. PLoS ONE 9(11): e111265.
https://doi.org/10.1371/journal.pone.0111265 Discussed at: https://vitamindstopscovid.info/01-supp/a-ratios/
07 McGregor R, Chauss D et al. An autocrine Vitamin D-driven Th1
shutdown program can be exploited for COVID-19. bioRxiv preprint.
2020-07-19 https://www.biorxiv.org/content/10.1101/2020.07.18.210161v1 Summarised and discussed at: https://aminotheory.com/cv19/icu/#2020-McGregor
08 Marik PE. Critical Care COVID-19 Protocol. 2020-12-07 https://www.evms.edu/covid-19/covid_care_for_clinicians/
09 Quraishi SA, Bittner EA, Blum L, Hutter MM, Camargo CA. Association
Between Preoperative 25-Hydroxyvitamin D Level and Hospital-Acquired
Infections Following Roux-en-Y Gastric Bypass Surgery. JAMA Surg.
2014;149(2):112–118. https://jamanetwork.com/journals/jamasurgery/fullarticle/1782085 Discussed at: https://vitamindstopscovid.info/02-autocrine/
10 Charoenngam N, Shirvani A, Holick MF. Vitamin D and Its Potential
Benefit for the COVID-19 Pandemic, Endocrine Practice (2021), https://www.endocrinepractice.org/article/S1530-891X(21)00087-2/
11 Fig 1D in Raisi-Estabragh Z, McCracken C et al. Greater risk of
severe COVID-19 in Black, Asian and Minority Ethnic populations is not
explained by cardiometabolic, socioeconomic or behavioural factors, or
by 25(OH)-vitamin D status: study of 1326 cases from the UK Biobank,
Journal of Public Health, Volume 42, Issue 3, September 2020, Pages
451–460, https://doi.org/10.1093/pubmed/fdaa095
12 Darling A, Blackbourn D, Ahmadi K, Lanham-New, S. Very high
prevalence of 25-hydroxyvitamin D deficiency in 6433 UK South Asian
adults: Analysis of the UK Biobank Cohort. British Journal of Nutrition,
125(4), 448-459. https://doi.org/10.1017/S0007114520002779 , PDF.
13 Sutherland JP, Zhou A, Leach MJ, Elina Hyppönen. Differences and
determinants of vitamin D deficiency among UK biobank participants: A
cross-ethnic and socioeconomic study, Clinical Nutrition, 2020,ISSN 0261-5614. https://doi.org/10.1016/j.clnu.2020.11.019
14 Stagi S, Rigante D et al. Severe vitamin D deficiency in patients
with Kawasaki disease: a potential role in the risk to develop heart
vascular abnormalities?. Clin Rheumatol 35, 1865–1872 (2016). https://link.springer.com/article/10.1007/s10067-015-2970-6 (Paywalled.)
https://sci-hub.se/10.1007/s10067-015-2970-6 Discussed at: https://aminotheory.com/cv19/#2015-Stagi
15 Vanegas-Cedillo PE, Bello-Chavolla OY et al. Serum Vitamin D levels
are associated with increased COVID-19 severity and mortality
independent of visceral adiposity. medRxiv preprint
2021.03.12.21253490, https://www.medrxiv.org/content/10.1101/2021.03.12.21253490v2
16 Tuncay E, Gemcioglu M et al. A notable key for estimating the
severity of COVID-19: 25-hydroxyvitamin D status. Turkish Journal of
Biochemistry, vol. , no. , 2021. https://doi.org/10.1515/tjb-2020-0423
17 Castillo ME, Entrenas Costa ML et al. Effect of calcifediol treatment
and best available therapy versus best available therapy on intensive
care unit admission and mortality among patients hospitalized for
COVID-19: A pilot randomized clinical study. The Journal of Steroid
Biochemistry and Molecular Biology, Volume 203, 2020, 105751.
https://doi.org/10.1016/j.jsbmb.2020.105751 Discussed at: https://aminotheory.com/cv19/#2020-Castillo
18 Sune Negre JM, Azpitarte OI et al. Calcifediol Soft Capsules WIPO WO 2016/124724 Al 2016-08-11
https://patents.google.com/patent/WO2016124724A1/ Discussed at: https://aminotheory.com/cv19/#25plusD3 .
19 Pakistan's first 'Vitamin D Academy' inaugurated in Punjab 2021-04-02
https://www.samaa.tv/living/health/2021/04/pakistans-first-vitamin-d-academy-inaugurated-in-punjab/
20 Over 200 Scientists & Doctors Call For Increased Vitamin D Use To
Combat COVID-19, Scientific evidence indicates vitamin D reduces
infections & deaths. https://vitamindforall.org